The post Shoulder Injuries appeared first on MetaMed.
]]>The shoulder is a complex joint, made up of many small muscles (rotator cuff, NOT rotor cuff) that all have a crucial role to play. ‘Crucial’ because the joint is so mobile and has little in the way of supporting ligaments, so the muscles have to be strong to stop your arm flapping about in the wind. If one of these muscles is out of kilter, you are more susceptible to injury and on-going pain. So, a quick anatomy lesson.
Shoulder anatomy 101
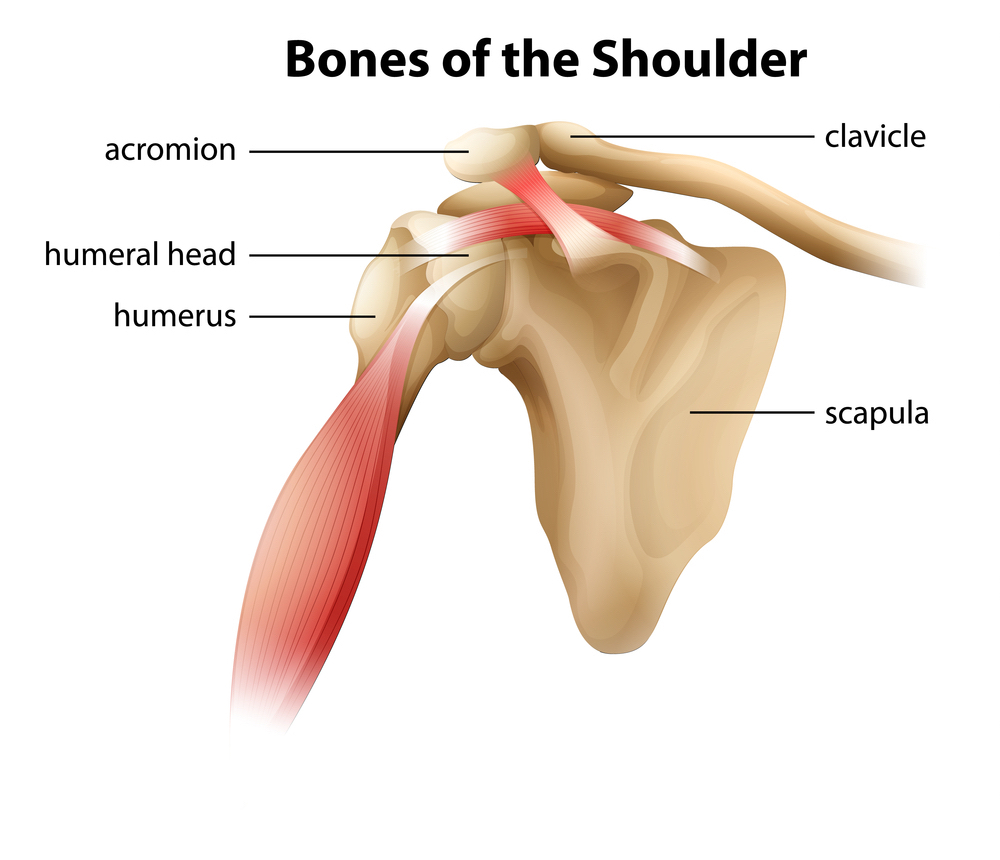
BONES: The shoulder complex is made up of 4 main bones, your humerus, scapula, clavicle and sternum. These combine to make 4 joints that all affect how your arm moves.
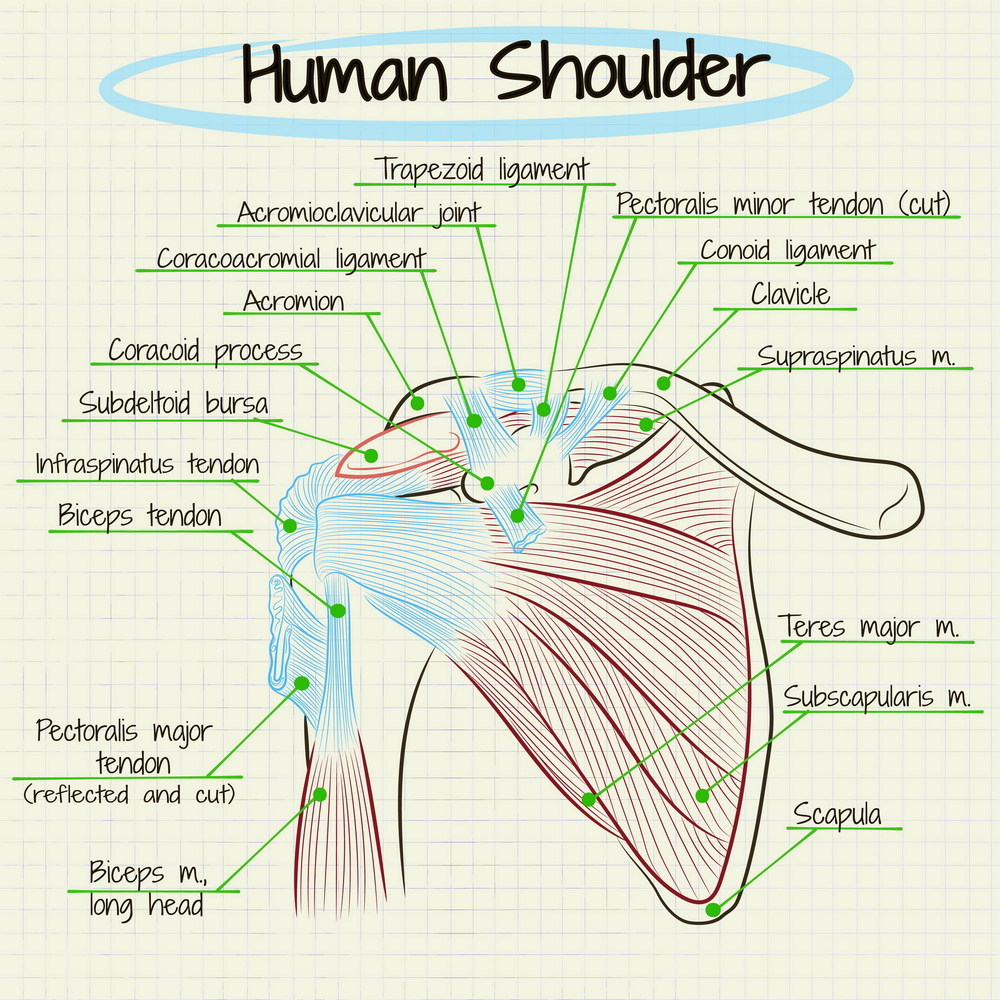
LIGAMENTS: The ligaments in the shoulder are small, this allows us increased mobility but sacrifices stability.
MUSCLES: This infamous structure is a collection of 4 muscles: subscapularis, infraspinatus, supraspinatus and teres minor. Good names huh? That’s why we call it the rotator cuff… These muscles are located on the back of your shoulder, with your pectoralis major and deltoid supporting the front.
Rotator cuff tear
What it is – The four muscles that make up the rotator cuff are responsible for keeping the ‘ball in the socket’ and assists in moving your arm. The leading cause of shoulder pain and disability, rotator cuff tears are common in sportspeople and those who do a lot of overhead work. They can be from traumatic injuries or from micro-tears that build up over time and lead to degenerative changes.
What it feels like – pain at night, with overhead activities, weakness and stiffness in the shoulder. Difficulty raising your arm, compensating by hiking through your upper traps in your shoulder. Pain can also radiate down the arm and into the neck.
Treatment
Manual therapy – works on muscle tension that may be affecting the position and mobility of the shoulder blade and humerus causing increased pain at the area. Exercises to strengthen the un-injured muscles and increase stability. Once the injured tendon has healed, focus is put on regaining the ability to activate and strengthen that muscle.
Medical – surgery to reattach the tendon, for complete or large partial tearsonly. This requires a referral to a specialist which your osteopath can organise. Receiving medical treatment before surgery is always a good option to improve your surgery outcomes. Surgery will also depend on how much you use your shoulder in work and sports. Over time your body can compensate even if a muscle or tendon has completely ruptured.
Other – ice/heat, rest, time.
Rotator cuff tendinopathy:
What it is – every muscle is connected to bone via a tendon. Tendinopathy occurs when there is a period of overuse, or increased compression or load. The tendon that is placed under strain fails to fully heal and the result is a swollen and vulnerable structure.
What it feels like – Dull pain that increases over time. Sometimes sharp pain/pinch in the shoulder or lifting your arm overhead. Growing weakness and pain with arm movement/sleeping on it.
Treatment
Manual therapy: Massage to reduce swelling and improve function in the muscle. Injury specific exercises. Advice on asymmetries in training/movement. Strengthening work to ensure other muscles around your shoulder are strong and supportive.
Medical: corticosteroid injections (often doesn’t last for more than a month). If you do opt for this try and get a guided injection to ensure the right spot is targeted.
Other: anti-inflammatories such as ibuprofen. Ice to reduce swelling. Rest from aggravating activities.
Shoulder impingement
What it is – There is a small space (approx. 1cm) underneath your clavicle and scapula called the acromioclavicular joint (see above). In the space runs the tendon to one of the rotator cuff muscles – Supraspinatus. Along with this tendon is a pad called a bursa, which helps the tendon to glide back and forth smoothly. If either of these get irritated (such as tendinopathy or bursitis) and swell up, the tissues get compressed into the small space and cause pain.
What it feels like – pain in the front of side of the shoulder that increases when the arm is lifted. Increased tension in the neck and increased headache frequency.
Treatment
Manual therapy: Conservative treatment of this injury can take up to a year in some cases however a decrease in symptoms is often noticed much sooner. It involves reducing tension in the shoulder/back/neck to encourage optimal function of the muscles and function of the joints. Guided rehabilitation and techniques to increase the space are also provided as well as improving overall strength.
Medical: corticosteroid injection but only once manual therapy options have been exhausted.
Other: rest from overhead activities, shockwave or laser therapy.
Dislocation/instability
What it is – Considering the anatomy explained above, with the lack of ligament and muscle support in the front of the shoulder, it’s no wonder that shoulders frequently dislocated forward (97% of all dislocations). This often occurs when the arm is stretched up in a reaching position. Instability occurs after a dislocation is the surrounding supporting structures have been stretched or torn, allowing the ball joint to ‘pop out’ easily. Nerve and rotator cuff damage can also occur.
What it feels like – If dislocated all movements are painful and the top of the humerus look misplaced. You'll be very limited with your range until the shoulder is relocated. Often people experience dislocations that spontaneously relocate by themselves. This instability can cause the shoulder to ache, feel loose, or vulnerable in positions such as reaching up or reaching up and back.
Treatment
Manual therapy: to help ease any muscular spasms and tension that has developed due to pain in the shoulder. This sets you up well for rehab.
Medical: relocation of joint, surgery to restore stretched/torn structures. Surgery can generally wait until the shoulder has been assessed.
Immobilisation: 3-6 weeks if under the age of 40 and 1-2 weeks if over the age of 40.
Restore motion: Work on slowly restoring full range of motion in the shoulder with specific functional exercises.
Strengthening: exercises introduced to prepare the muscles for a full return to sport/work.
The importance of rehab
As you can see, these injuries often have a long rehab process that requires a combined effort from patient and their manual therapist, with specific exercises and treatments. The amount of effort you put into your rehab, whether it be resting (actually resting) or doing the exercises prescribed, the faster you will be pain free.
If you have a sore shoulder that’s just not going away, book in with one of our practitioners today for an assessment. We are here to help!
The post Shoulder Injuries appeared first on MetaMed.
]]>The post Breathing Well appeared first on MetaMed.
]]>Why Learning to do it Properly is so Important
It is something we all do thousands of times every day. Whether we are awake or asleep, resting or active; to breathe is to be alive. Whilst most of us don’t take much notice of our breathing, there are a few very important reasons why we should.
- Improves blood flow
- Improves energy
- Supports a strong immune system
- Alleviates stress
Let's just touch on one of the issues most people have in life and how improving your breathing can help.
Stress response
We’ve all been told at one time or another to “take a deep breath” when we have been feeling stressed. As unhelpful and annoying as this can be at the time, there is some sense behind this.
Our “fight or flight” instinct, also known as our body’s stress response, is how we decide to confront or avoid danger. When we breathe in deeply our lungs expand and compress the walls of the heart, restricting blood flow. To compensate, our heart rate increases stimulating this fight or flight stress response.
When we breathe out, the pressure in the thoracic cavity drops and the body relaxes! So, in short, it is the exhale that truly helps us relax, not taking a deep breath in!
This brings us to an issue we see regularly in clinic – people holding their breath in, or not breathing out fully. It's usually the first change when stress is encountered – holding your breath. Over time if we continue this pattern we can keep our body in the ‘fight or flight' response. Stress and anxiety anyone? No thanks.

One Simple Trick to Alleviate Stress
Next time you feel stressed or anxious make a mental note of your breathing. Are you holding your breath? Are your lungs full and chest tight? Taking a moment to forcefully exhale several times can make a big difference and quickly reduce the fight or flight response.
Try This Breathing Technique
Inna Kahzan of Harvard medical school recommends that 40% of the breath cycle is for inhaling, and 60% is for exhaling – so for a 4 second breath in, take 6 to exhale. This ensures not only a full exhale, but also slows the breathing, avoiding risks of hyperventilation which can make that stress response much worse.

Two Ways to Breathe
- Belly breathing
- Upper chest breathing
While breathing is mostly automatic, every breath is not identical. Diaphragmatic (AKA belly breathing) is best for keeping that stress response to a minimum, but unfortunately the stresses of day to day life can lead us to quickly fall into a habit of breathing into the upper chest. This is not ideal, and aside from typically shallower breathing, it can also cause tightening of muscles in the front of the neck and chest over time. If you catch yourself doing this remember the 40/60 rule and EXHALE for longer!
The stress response/breathing relationship is cyclical, so busy lifestyles often feed into poor breathing patterns. However habits form young, and breathing is no exception either. Some of our cultural expectations, such as the wish to have a flat tummy, means we learn from an early age to hold our stomach muscles in tight.
As I’m writing this, I’m trying to breathe deeply into my belly whilst hunched over my desk (like many who work in an office) – try it, it’s practically impossible. This is another great example of the importance of breathing and taking time away from the desk every so often.

If you know poor breathing habits may be contributing to your pain or symptoms come and visit one of our practitioners. If you're unsure we're more than happy to book in a 15 minute complimentary chat to see if we can help you.
Alternatively, if you're not anywhere near Wanaka or Queenstown we also love Emma Ferris the breathing physio from The Breath Effect. She has a great online course and more information on how to retrain your breathing. Click here to find out more information.
The post Breathing Well appeared first on MetaMed.
]]>The post Imaging – Help or Hindrance? appeared first on MetaMed.
]]>Modern Day Medical Imaging.
Modern imaging techniques such as X-ray, ultrasound, MRI and CT Scans have the ability to show us anatomical structures in great detail. Since the inception of medical imaging, vast improvements have been made on clarity and availability; providing medical practitioners and patients with a clear diagnosis. A clear diagnosis can help to guide practitioners to give you a clear prognosis and management plan, whether this is a broken bone, internal bleeding, head trauma, or a tumour.
My Experience
After recently breaking my wrist (again) and going in for an x-ray, I realised that many would not be aware of the risk associated with x-ray and CT scans. Had I not known this already, I would be completely unaware that a single x-ray can increase your risk of cancer (1). CT scans are also problematic, with even higher levels of radiation. Areas such as arms and legs require a much lower radiation strength and therefore the risk is less. However, the spine or chest with its many layers of bone, muscle and organ require a higher strength scan, resulting in increased risk (1). Fortunately, ultrasound and MRI scans are safe. However, ultrasound cannot read bones, and MRI is very costly.

Hunting For A Diagnosis
When in pain, the desire to get a diagnosis is strong. For example, those with an old shoulder injury that just won’t heal will often go to their doctors pleading for an x-ray or ultrasound. Similarly, back pain can be debilitating and those suffering become desperate for an answer. However, you have to weigh up the pros and cons. What benefit will come from getting a diagnosis? Once you have a diagnosis – will your management options change?
Does Getting An Image Change Treatment?
Have you been diagnosed with shoulder impingement or tendinopathy? Have you been scanned, given the injection and in 8 weeks’ time the pain has come back? Here, the treatment you would receive from an Osteopath would be the same pre and post-scan/injection – the management doesn't change. Osteopaths use a variety of diagnostic tools including the same active tests a specialist would use, considering the injury cause and looking at your individualised anatomical makeup. In doing so we can diagnose and treat with great results and no unnecessary scans or injections required.

Here's An Example
The Conservative/Treatment Path
Shoulder pain or back pain are great examples of injuries that should be treated conservatively initially. ‘Conservative treatment’ includes seeing your local Osteopath, Acupuncturist or Physiotherapist for treatment, taking recommended supplements, attacking an exercise regime with focus by regularly doing the stretches provided.

The Specialist Path
The non-conservative pathway is seeing a specialist, getting a scan and putting a name to your disorder. The specialist will likely recommend getting a corticosteroid injection, nerve block injection or having surgery. These treatment options are invasive, have varying results and don’t address the reason why the injury happened in the first place (2–4). Not to mention the side-effects of steroid injections; steroid injections have been found to slow healing in the tendon (5).
What The Studies Show
Over imaging is an endemic in healthcare. Studies have shown that unnecessary imaging and diagnosis hunting can lead to poorer health outcomes and higher levels of disability (6). There is growing evidence that pain has a strong association with stress levels, poor sleep, anxiety/depression and negative beliefs around pain. Indicating that all aspects of your life need to be addressed when treating pain – something we strive to do at MetaMed. We help guide you to de-stress, sleep better and become more trusting of your body and its strength, resulting in a more positive future outlook. We actively refer within the community to find you the right trainer/practitioner to support you back to feeling 100%.
To Sum It All Up
Getting a diagnosis from medical imaging is not the be-all and end all to your issue. Studies have shown that people who are pain-free often have ‘abnormal’ findings when given an MRI. In this study 91% had disc degeneration (loss of height in your spinal discs), 56% had disc bulges, 32% had disc protrusions and 38% had annular tears (the ligament around the spinal disc) (6). Yet these people all reported no back pain. Similarly, people with shoulder impingement, bursitis or tendinopathy often have similar if not worse findings on the unaffected side. When scanned, 95% of asymptomatic patients were found to have ‘abnormal’ findings in their shoulders (7). Which leads us to the conclusion that the pain you feel doesn’t necessarily correspond to the ‘abnormal’ findings that imaging may provide. In these cases, one may get little or short-lasting relief from nerve blocks, steroid injections or surgeries.

The main takeaway message here is before you go searching for a diagnosis, as it can have a negative impact on your health. Instead, give the conservative treatment a try. Focus on what combination of treatment/exercise makes you feel better. Radiological imaging should only be used when there are clear indications to do so and once conservative treatment options have been exhausted.
Written by Anna Burgess, Osteopath @ MetaMed · WANAKA
References
1. Harvard Medical School. Radiation risk from medical imaging – Harvard Health [Internet]. 2018 [cited 2019 Jan 30]. Available from: https://www.health.harvard.edu/cancer/radiation-risk-from-medical-imaging
2. Cook T, Minns Lowe C, Maybury M, Lewis JS. Are corticosteroid injections more beneficial than anaesthetic injections alone in the management of rotator cuff-related shoulder pain? A systematic review. Br J Sports Med [Internet]. 2018 Apr 1 [cited 2019 Jan 30];52(8):497–504. Available from: http://www.ncbi.nlm.nih.gov/pubmed/29305377
3. Carofino B, Chowaniec DM, McCarthy MB, Bradley JP, Delaronde S, Beitzel K, et al. Corticosteroids and local anesthetics decrease positive effects of platelet-rich plasma: an in vitro study on human tendon cells. Arthroscopy [Internet]. 2012 May [cited 2019 Jan 30];28(5):711–9. Available from: http://www.ncbi.nlm.nih.gov/pubmed/22264830
4. Jordan JL, Konstantinou K, O’Dowd J. Herniated lumbar disc: injection interventions for sciatica. BMJ Clin Evid [Internet]. 2016 [cited 2019 Jan 30];1118. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4747321/
5. Coombes BK, Bisset L, Vicenzino B. Efficacy and safety of corticosteroid injections and other injections for management of tendinopathy : a systematic review of randomised controlled trials. Lancet [Internet]. 2010;376(9754):1751–67. Available from: http://dx.doi.org/10.1016/S0140-6736(10)61160-9
6. O’Sullivan P, Lin I. Acute low back pain: Beyond drug therapies. Pain Manag Todayanagement Today. 2014;1(1):8–13.
7. Girish G, Lobo LG, Jacobson JA, Morag Y, Miller B, Jamadar DA. Ultrasound of the Shoulder: Asymptomatic Findings in Men. Am J Roentgenol [Internet]. 2011 Oct 20 [cited 2019 Jan 31];197(4):W713–9. Available from: http://www.ajronline.org/doi/10.2214/AJR.11.6971
The post Imaging – Help or Hindrance? appeared first on MetaMed.
]]>