The post Osteopathic Treatment For The Feet – Does it Work? appeared first on MetaMed.
]]>Your Feet – A Primer
Each foot is made up of 26 bones and 33 individual joints. It’s the foundation of every single movement we do when standing. The dozens of muscles and ligaments in each foot serve to maintain balance and stability through our only contact point to the ground. The feet are not just inert extensions of our lower limbs, they are the vital platform for almost all of our movement, and should be cared for just like any other area when it comes to injury and prevention.
What kind of ankle and foot problems does an Osteopath treat?
The following conditions affecting the foot can be effectively treated by your osteopath
Plantar Fasciitis
A potentially very painful condition that usually begins as a pulling feeling in the heel or the arch of the foot. This quickly turns into a sharp pain which is often worse in the morning or when initially standing up. It’s a complicated and unique condition that is often misunderstood, and therefore often persists for many months. Fortunately, there are many things we can do to help recover faster and even help prevent plantar fasciitis in the first place.
- Avoid standing for prolonged periods, especially on solid floors like concrete. Many workplaces with solid floors now have rubber matting which can help reduce the fatigue of the foot muscles.
- When standing is unavoidable, the right shoes are essential. You should choose a shoe with a softer sole and arch support to suit your foot. If you’ve got particularly high or flattened arches then orthotic inserts may also be useful.
How to treat Plantar Fasciitis
The best way of treating Plantar Fasciitis is to catch it early. 95% of patients will recover well with conservative treatments that include stretching and strengthening. Depending on what biomechanical issues, issues can be limited to the foot. But problems with the knees or hips can have knock-on effects over time and so these areas should be addressed as well.
You’ll likely also need to make some temporary changes to your daily activities to reduce the strain on the foot. At home, icing the sole of the foot can feel great and give some immediate relief. Keep a bottle of water in the freezer and use it to roll the sole of your foot over it for 15-20 minutes.

Achilles Tendonitis
More accurately called Achilles Tendinopathy, this is a type of overuse injury in which inflammation is not a big factor. With Achilles Tendinopathy, the tendon struggles to repair itself fast enough. You feel pain either directly on the heel or just above the heel where the tendon joins the calf muscles. You might feel the tendon is thicker in this area compared to the other side, or you might find a small nodule. Nodules come from poor collagen organisation as the injury struggles to heal. This happens when the tendon is being stressed more than usual. For example, rapidly increasing running distances, increased hill running, overtraining, or poor footwear. Biomechanics can also play a part if you have poor knee, hip or ankle stability, or chronically weak muscles/tendons in the first place.
How to Treat Achilles Tendinopathy
Fortunately, tendinopathies can be treated successfully. Recovery is faster when the injury is managed correctly at an early stage. Initially, there will need to be a period of rest followed by progressive and very specific strengthening exercises. Then the underlying biomechanical issue should be addressed – a vital part of prevention. Continuing to run/jump/overwork your tendon can lead to irreversible changes, degeneration and weakening of the tendon, and is a precursor to a full tendon rupture!
Sprains
Ankle sprains and foot sprains are one of the most common types of injuries. Most active people will have rolled their ankle a few times in their lifetime. It can take quite a while to recover. Each sprain will reduce the amount of stability, making it more and more likely that you’ll sprain it again. And this can lead to chronic ankle instability.
A serious ankle sprain can overstretch the ligaments and can sometimes stretch the tendons around it. The more they stretch, the less stable your ankle will be. Properly diagnosing and treating an ankle sprain in a timely manner is vital to avoid long term complications, re-sprains, and chronic ankle pain. Your rehab will include a lot of strength and balance work to regain proprioception which is absolutely vital for a strong and stable foot.
Heel Pain
Heel pain can have a variety of causes and they all need to be treated specifically. Your pain might have crept up gradually, or might be after an impact or a sprain, but either way, it can be one of the most annoying places to hurt. Possible causes of heel pain include stress fractures, heel spurs, bursitis, or a ruptured fat pad, but by far the 2 most common causes are Achilles Tendinopathy and Plantar Fasciitis.

Trapped Nerve
A trapped nerve can happen in any part of the body. The following are the most common kinds of issues caused by trapped nerves in the foot or ankle.
Tarsal tunnel syndrome
In this painful condition, the Tibial Nerve is compressed and irritated as it goes into the foot. It runs down on the inside ankle, between your ankle bone and another smaller bone, and is held in place by a big ligament – creating a kind of tunnel that it passes through (hence the name). This nerve can get compressed from injuries, such as sprains or fractures, or it can happen over time.
Flat-footed individuals are at risk because the outward tilting of the heel can strain the tarsal tunnel and put pressure on the nerve. Typical symptoms of this nerve entrapment are tingling, burning, pain or pins and needles. Usually, this is felt on the inside of the ankle or the bottom of the foot.
Plantar nerve entrapment
This issue is less common than other trapped nerves and can feel very similar to plantar fasciitis. The main difference is that nerve pain tends not to improve at rest and can increase intensity at night. There is usually chronic burning heel pain which is made worse with stretching and standing.
Morton’s Neuroma
A unique and fairly common condition which is often described as feeling like you have a stone in your shoe. This is caused by a small growth around a nerve between your 3rd and 4th toe, just below the point at which your toes separate from the rest of your foot. Whilst this condition can be quite uncomfortable, it is rarely painful. It’s more likely to affect women as it is often caused by compression of the nerve by tight narrow shoes or high heels.
Gout
Gout is a pain kind of arthritis that can affect any joints (but usually the big toe). It will come on quite quickly and present itself as swelling, redness and extreme tenderness in the affected area. It occurs when the body has excess uric acid in the blood causing tiny sharp crystals to form in and around joints. Usually the body will absorb uric acid naturally, but diets high in red meat, seafood, organ meats, and alcohols such as beer, can increase the uric acid levels.
Other risk factors include obesity, kidney disease, untreated high blood pressure, family history, and being a male age 30-50. Those who are disposed to it can have repeated attacks over the years. Each of which might last anywhere from a few days to a few weeks. Prevention is much easier than treatment for this condition as it usually relies on anti-inflammatories and allowing the uric acid crystals enough time to be re-absorbed by the body.
How do Osteopaths treat foot pain?
It should go without saying that the most important element to treating the foot and ankle is getting the right diagnosis! Most conditions have very specific needs when it comes to recovery, but there are a number of things that an osteopath will usually consider regardless of the type of injury:
- Movement: Does the foot move like it should? Does it move too much? Simple questions give us big clues about how your joints and muscles will are functioning. A hypermobile joint might mean instability or indicate previous sprains. A restricted joint could be a result of a dysfunction in your gait. Knowing how your joints move gives us an idea of which parts have been under increased load. We can then use a range of techniques including gentle manipulation (cracking) to increase mobility, or alternatively help you strengthen weaker areas.
- Muscles: In the ankle, muscles play a vital role in balance and stability; they make the micro-movements to keep us standing upright. But these muscles are prone to injury whenever the foot or ankle is injured too. We use a combination of soft tissue techniques, cupping, dry needling, and stretching, as well as using exercises to build strength and balance.
- Compensation from other areas: Issues further up the leg can cause real issues for the foot. For example, a hip rotated outward makes it nearly impossible to walk naturally. Ultimately, it’s your foot that has to take make the compensation because it’s the only contact point to the ground. With most foot/ankle injuries, osteopaths check the knees, hips, pelvis and lower back as well.
- How you stand: Looking at how you stand or walk is a great way to see how your body functions as a whole. Biomechanical issues can be hard to spot when you remain still so your osteopath will ask you to do a range of movements and see how the leg integrates and works together. The aim is to take any unnecessary pressure from the injured area by ensuring you are moving biomechanically as well as possible.
- Your day-to-day life: The goal is to get you back to doing what you love as quickly as possible. So osteopaths will always try to find a way to keep you active through your recovery. This might be through certain activities, specific rehab exercises, or even modifying existing activities to help you avoid aggravating your injury. Your osteopath will advise on the best way to continue working and how to avoid making your injury worse by doing so.
The post Osteopathic Treatment For The Feet – Does it Work? appeared first on MetaMed.
]]>The post Soft Tissue Injury Treatments: Your Options appeared first on MetaMed.
]]>Chronic soft tissue injuries
These types of injury are the result of repetitive stress on a tissue. Commonly known as overuse injuries. See our Tendinopathy post for more details.
Signs and symptoms
Different soft tissue injuries have different signs and symptoms but there is usually some level of redness and swelling, as well as pain and reduced range of motion. There may be some bruising.
Joint-stabilising ligament injuries
Ligament injuries range from mild tearing of a few fibres to complete tears, which can lead to joint instability. The common areas affected are the knee and ankle, but it can also happen around the shoulder, elbow and wrist.
Ligament injuries are graded from 1-3:
- Minor injury with little swelling and tenderness: minor impact on function due to intermittent pain on movement. Grade 1 usually heals in a few weeks, with max strength returning after 6 weeks.
- Ligaments are stretched but intact: some joint laxity (giving way) may be experienced as well as moderate swelling pain and negative impact on function. Grade 2 requires some reduction in use to offload the tissue during the initial phase. Healing may take anywhere from 6 to 12 weeks depending on the injury.
- Complete ligament rupture with excessive joint laxity: Often painful but can also be pain-free due to the destruction of sensory fibers in the injury. Marked swelling and bruising. Painful or inability to weight-bear. Grade 3 requires the opinion of an orthopedic specialist to determine if it requires surgery. A return to normal activity can take anywhere from 4 to 12 months
Muscle Strains
Muscle strains are the same as ligament sprains but in a different type of tissue in the body. Strains happen when a muscle is overloaded and fails, causing tearing of the fibres. We grade muscle strains in the same way as ligaments, from one (mild) to three (severe). Symptoms include swelling, bruising, redness, pain at rest and with movement, inability to use the muscle (moderate to severe only), and muscle weakness.
Treatments for muscle strains depend on the severity of the injury. Initially, POLICE protocol (see below) should be followed. An assessment and accurate diagnosis by an osteopath or physiotherapist will help to determine when and how the muscle can safely be loaded again. The initial rehab starts with low impact movements, followed by a gradual increase in tension. Proprioception and endurance training is recommended only in the advanced rehab stages.
Tendon Injury
Tendons connect muscles to bones and work to transmit forces between the two. The most common tendon pain is from overuse – called tendinopathy. However, acute tendon ruptures also occur.
Tendon ruptures often happen without warning or apparently for no particular reason. The most frequently injured tendons are covered below. A ‘pop’ or a ‘bang’ followed by weakness and pain, is a common sign that a complete rupture has happened. These commonly happen in the achilles in the ankle and the bicep tendon in the upper arm.
Rotator cuff tendon injuries are categorised based on which of the four rotator cuff tendons is affected and the extent of the injury – small/medium/large/complete tear. Symptoms include severe pain at the time of injury, night pain, pain with overhead movements, pain radiating down the arm, and shoulder muscle weakness.
Full-thickness tears require surgical intervention, however, in most other cases conservative rehab is recommended – such as osteopathy, physiotherapy, or acupuncture and specific exercises and stretches.
Bicep tendon injuries often occur after a strong, sudden contraction of the bicep muscle. Similar to the rotator cuff, symptoms include pain in the front of the shoulder, pain with overhead movements, night pain and ‘pop-eye deformity’ – when the bicep muscle, under contraction, appears to rise lower down the arm.
Surgery is generally offered to younger patients that are athletic or require maximal arm strength – Tradesmen, for example. Conservative management is recommended.
A Quadriceps tendon rupture means you will be unable to straighten the knee without help. Some people can walk after injury, some cannot. Graded as either partial or complete.
Partial ruptures require a short period of immobilisation (possibly in a moon-boot) followed by a gradual return to normal activities with specific strengthening exercises. 3-6 week heal time.
A complete rupture calls for surgery, usually in the 72hrs following injury, to reattach the tendon. Following surgery is a period of immobilisation. Depending on the patient and surgeon, rehab will either be conservative (around 4-6 weeks immobilisation) or aggressive (around 10 days immobilisation with exercises included early on). The aggressive approach has produced better results more quickly but it is not for everyone.
People with Achilles injuries often report that the injury felt like someone kicked/stabbed them in the leg, accompanied by a ‘bang’. Other symptoms include swelling in the back of the heel, decreased ability to heel raise or point toes and a palpable gap in the tendon. Achilles injuries are graded 1-4:
- Grade 1: partial ruptures, less than 50% – typically treated with exercises and manual therapy.
- Grade 2: complete rupture with tendinous gap ≤ 3 cm – typically treated with surgery
- Grade 3: complete rupture with tendinous gap 3 to 6 cm – surgery required
- Grade 4: complete rupture with a defect of > 6 cm (neglected ruptures) – surgery required
Rehabilitation
Like the different signs and symptoms, there are also different rehab stages depending on the severity of your injury. Seeking professional guidance after a soft tissue injury will help you to reach your recovery goals faster. Injury specific exercises, massage, joint mobilisation and natural pain relief will speed up recovery and help prevent re-injury.

At-home care
Everyone has heard of RICE: Rest, Ice, Compress, Elevate.
However, I’d like to introduce a new mnemonic, POLICE: Protect, Optimum Loading, Ice, Compression, Elevate.
- P: Protect yourself from further damage by taking an appropriate amount of time off. Have the injury assessed by a professional to find out how long you should rest and when you can return to daily activities.
- O + L: “Optimal Loading” helps to encourage tissue healing, stimulating repair and building strength in the damaged tissue so it can cope with the strains placed on it when you return to your sport/work. Graded loading helps to prevent stiffness, reduce swelling, and reduce pain. Loading an injury is a key element in producing strong tissue that can handle the forces you place on it. This helps prevent future injury.
- I: Ice. Cryotherapy causes the blood vessels in the area to tighten and in doing so reduces swelling, while also reducing inflammation. However, inflammation is part of the natural healing process after a traumatic injury. Icing an injury for long periods of time can cause further tissue damage and prevent optimum healing. We recommend using an ice pack for 10mins at a time, then having a break and coming back to it again in an hour. Remember to wrap your ice pack in a damp towel or cloth to minimise skin irritation.
- C: Compression also helps to reduce swelling and any bleeding at the injury site. A compression bandage (tubigrip) can provide comfort and support to an injury. It should not increase pain or be so tight that the area beneath it turns red/purple.
- E: Elevation increases the return of blood toward your heart, reducing swelling and easing pain by facilitating the removal of inflammation by-products that cause extra nerve sensitivity.
Frequently Asked Questions
What is the best treatment for a soft tissue injury?
This is highly variable and depends on the extent of the injury. What’s important is following the P.O.L.I.C.E protocol directly after the injury, seeking professional advice, and getting an accurate diagnosis.
How long does it take for a soft tissue injury to heal?
Factors that influence the recovery time include the age of the patient, the patient habits such as smoking, and adherence to the rehab protocol.
| Healing Times | |
| Delayed Onset Muscle Soreness (DOMS) | 0-3 days |
| Muscle strain | Grade 1: 0-2wks Grade 2: 4d-3mo Grade 3: 3wk-6mo |
| Ligament sprain | Grade 1: 0-3d Grade 2: 3wk-6mo Grade 3: 5wk-1yr |
| Tendon | Rupture: 5wk – 6mo Tendinopathy: 3wk-12mo |
| Bone | 5wk-3mo |
| Cartilage | 2mo-2yrs |
| Ligament graft | 2mo-2yrs |
Can soft tissue damage be permanent?
Yes. Some ruptures do not qualify for surgical repair and are therefore permanent. However, this is generally only the case when the patient is not in pain or surgeons determine that surgery would non-beneficial or non-successful. Most other soft tissue injuries will heal given the right time and rehab.
Is soft tissue damage painful?
Yes. However, patients often report feeling pain at first followed by a period of no pain when the tissue has fully ruptured.
Is heat good for soft tissue injury?
No. Heat is great for tired or spasmed muscles. Applying heat can also be used as an ice/heat flush if recommended by your health professional. However, acute/new soft tissue injuries should always have ice applied to help reduce inflammation and swelling.
Does massage help soft tissue damage?
Yes. But only after the initial acute phase has passed. Osteopathic treatment can help with repair and healing, reducing swelling, inflammation, pain from compensatory movements and addressing why the injury happened. Your Osteopath will also help to diagnose the injury and guide your rehabilitation. You will get back to your best, pain-free-self faster than if left alone.

The post Soft Tissue Injury Treatments: Your Options appeared first on MetaMed.
]]>The post Are Foam Rollers Worth it? Why & How to use a Massage Roller appeared first on MetaMed.
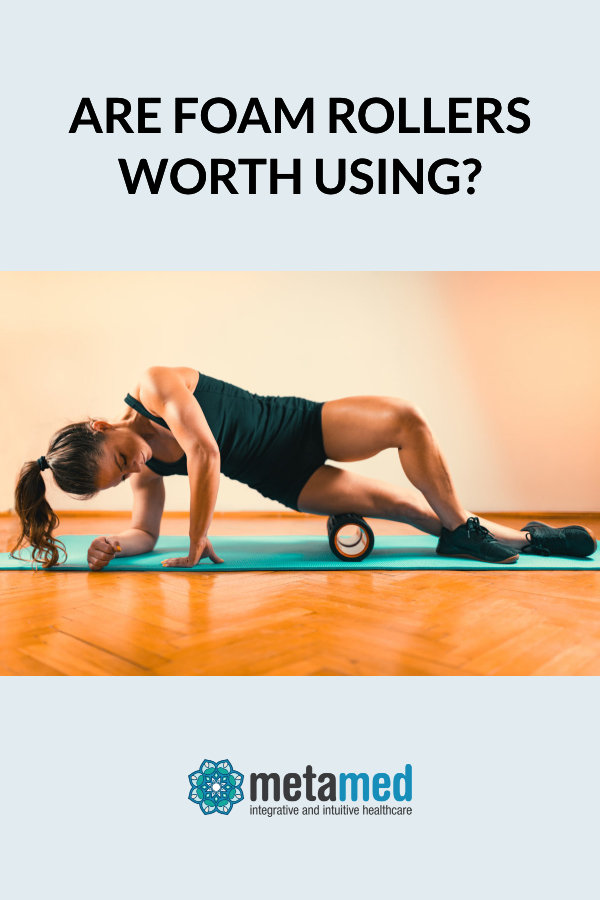
]]>Is foam rolling good for you?
Using foam rollers the correct way can help increase flexibility, improve joint range-of-motion, relieve back pain, improve blood flow, and help reduce muscles soreness from post-workout DOMS. These are all reported benefits from regular foam rolling. If you’ve been using a roller for a while, you’ll have already noticed the positive changes. You might also be wondering why so many people are torturing themselves in the name of health. But foam rolling should be no more painful than a firm massage. If you grit your teeth as you roll down your IT band for the hundredth time, stop right there. We’ll talk about how to use one properly but for now, let’s look at why you should use a roller.

Why should you be foam rolling?
- Flexibility – Foam rolling has been shown to significantly improve flexibility, especially when combined with a typical warm-up routine before exercise (1). And the good news is you don’t need to roll it ‘til it hurts; studies have shown this improvement after just 2 minutes of rolling the specific area (2). So whether you’re looking to work on the flexibility in yoga, or just looking to loosen those stiff joints, reaching for the foam roller is a good idea.
- Performance – When it comes to pre-workout warm-up, you might think back to school days of standing around doing a few static leg stretches. As it turns out, those static stretches actually reduce the endurance and strength of muscles immediately after stretching (3). Not ideal if you’re about to do a heavy set of squats! Fortunately, foam rolling has no such negative side effects! Next time you warm-up for the squat rack, try a few minutes of rolling the hip flexors, quads and glutes and leave the static stretching for after your workout.
- Recovery – Post-workout foam rolling has become a staple for many athletes and for good reason. Foam rolling has been shown to substantially reduce the amount of soreness associated with DOMS and help your muscles recover faster (4). That’s a Win-Win situation.

What about back pain?
Mild back pain is often due to overuse or and imbalance of muscles. For this sort of problem, foam rolling can be a great tool to help relieve tightness. However, there are many reasons for back pain and not all of them should be treated with the roller. Figuring out when you should and shouldn’t use a roller can be difficult. The best course of action is to check with your practitioner.
How do I use a foam roller?
This is a really common question. Luckily it’s not hard to learn how to use a foam roller. After consulting with your osteopath, they might recommend you foam target a particular muscle or muscle group. They can show you exactly how to “roll” these areas. (At MetaMed, we have some handy printouts with diagrams in case you forget).
CLICK HERE TO GET YOUR FOAM ROLLER EXERCISES
When rolling any part of the body, there is a sweet spot of pressure for the best results; too much or too little and you won’t get the maximum benefit. All parts of the body are not equally receptive. Some areas can have trigger points or tighter muscles that can feel more painful than others.
We recommend finding a pressure you can work with for 2 minutes. It should allow you to relax. Your muscles will be tight when you begin but should relax by the time you’ve finished. If not, and you’re still feeling discomfort, you might be using too much pressure. In terms of frequency and duration, 3 to 4 times a week works for most people and approximately 2-3 minutes for each area.
I’m a runner, do I need to roll more often than most?
Runners will benefit from around 3 times a week but avid runners doing long-distance training might want to get an extra rolling session done. Pay attention to the IT band. Many runners live in fear of IT band syndrome. This painful condition affects the knee and sometimes the hip. Pain is felt when the IT band rubs over bony areas, causing inflammation during the running motion. The syndrome is often associated with tightness of the IT band. In the early days of foam rolling, this thinking led to runners spending hours a week rolling up and down this painful band of tissue.
While more rolling may sound like a good idea, the reason we call it a “band” and not a muscle is because it’s simply not a muscle. In fact, it’s technically a tendon. And tendons can’t be stretched. If you’re worried about ITB syndrome or already have it, there are ways to address it without torturing yourself on the roller!

What kind of roller do I need?
Foam rollers come in a variety of sizes, textures, and densities. Like most products these days there is an abundance of choice. We recommend picking a medium-soft one for beginners with a relatively smooth surface. Experienced users might prefer firmer ones that can come with spikes and nodules that help get into the hard-to-reach places. Note that these products can be seriously uncomfortable for the majority of people.
Is there anything I should watch out for when using my roller?
On the whole, foam rolling is a very safe practice provided it’s used carefully. Roll muscles only. Avoid bony bits, rolling over joints, or the site of a recent injury. If it’s really sore or painful, stop and ask us about it!
- Mohr, A., Long, B. and Goad, C. (2014). Effect of Foam Rolling and Static Stretching on Passive Hip-Flexion Range of Motion. Journal of Sport Rehabilitation, 23(4), pp.296-299.
- MacDonald, G., Penney, M., Mullaley, M., Cuconato, A., Drake, C., Behm, D. and Button, D. (2013). An Acute Bout of Self-Myofascial Release Increases Range of Motion Without a Subsequent Decrease in Muscle Activation or Force. Journal of Strength and Conditioning Research, 27(3), pp.812-821.
- NELSON, A., KOKKONEN, J. and ARNALL, D. (2005). ACUTE MUSCLE STRETCHING INHIBITS MUSCLE STRENGTH ENDURANCE PERFORMANCE. Journal of Strength and Conditioning Research, 19(2), pp.338-343.
- Lane, J., Kripaitis, D. and Spina, M. (2017). The effect of Foam Rolling (FR) on recovery from delayed onset muscle soreness. Physiotherapy, 103, p.e46.
Foam roller
The post Are Foam Rollers Worth it? Why & How to use a Massage Roller appeared first on MetaMed.
]]>The post Plantar Fasciitis Treatment: Your Options in New Zealand appeared first on MetaMed.
]]>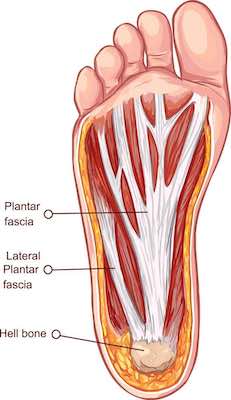
Plantar fasciitis is a unique repetitive strain injury affecting people from all walks of life: runners, walkers, even people who have to stand on hard surfaces at work especially on concrete floors.
For some, plantar fasciitis can be resolved in a matter of weeks, for others it can be one of the most stubborn and frustrating conditions out there. Part of the problem is that it is still a bit of a medical puzzle.
What are the symptoms?
Most people first notice a tightness or a pulling sensation in either the arch of the foot, the heel or both. This can quickly become a very sharp pain felt in the heel, and often much worse in the morning, or when standing up after having been sitting for a while. You might find the foot eases a bit as you walk around, especially in the early stage, but as it progresses, you might find that any weight-bearing on your feet is pretty darn horrible!
What aggravates plantar fasciitis?
The causes are not particularly straightforward. Whilst there will be some of the inflammation in the early days, plantar fasciitis is not a chronic inflammatory condition, despite what the name implies (“-itis” usually means inflammation).
It’s a bit like tendonosis crossed with some degeneration of the plantar fascia. It’s an overuse injury, and it’s common in runners (and menopausal women). Plantar fasciitis is caused by too-much repeated load on the arch of the foot leading to tissue fatigue, but biological and biomechanical factors are also involved. Not everyone who runs a lot will suffer from it.
The plantar fascia is like a web. Or to think of it another way, it’s like a bowstring (with the arch of the foot being the bow itself). Along with a few muscles it supports your foot mechanics and helps maintain the shape of the foot and allows it to be “springy” – very important for running. Too much stretch and it can stretch out and fatigue, too little and it won’t be able to absorb the forces from the ground very well; either way it won’t cope with the strain!
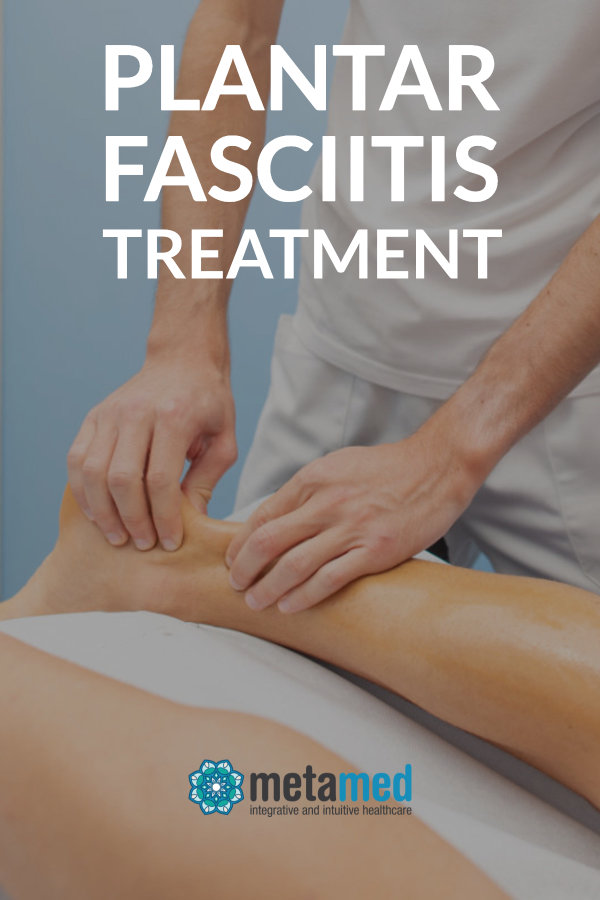
What’s the best way to treat plantar fasciitis?
Plantar fasciitis is a sore and incredibly frustrating condition to have. The good news is over 95% of people will recover with conservative treatment alone. This treatment will usually include a combination of manual therapy, stretching regimes, short-term use of anti-inflammatory drugs, and lifestyle/activity modification.
Surgical options that involve cutting part of the plantar fascia are generally reserved for the most severe and chronic cases. And this is why it’s important to see a professional quickly if you think you might be developing plantar fasciits. Do not wait until it becomes unbearable!
Can an osteopath help with foot problems?
Osteopaths assess the biomechanical components and the lifestyle factors that contribute to plantar fasciitis. They look at your day-to-day life, your footwear, your foot posture and stability, and your gait. The number priority one is reducing the load through the arch of your foot. An osteopath might recommend wearing a supportive shoe with good cushioning as your regular daily shoe – especially if you usually wear flat shoes, high heels or jandals.
It's common with plantar fasciitis that the issues aren't actually in the foot, but higher up, such as weakness in the hips that causes more strain on the foot.
If you’ve got a high arch, then it’s often good to get some orthotics for your shoes. Podiatrists can help you source insoles specifically made for your foot. With your footwear taken care of, you’ll probably have to make a few changes to your daily routine. This might mean taking a break from running for a while or taking the weight off your feet if you stand all day. If the pain is acute and it needs a little extra support, taping is another way to take the pressure off the medial arch.

How to Treat Plantar Fasciitis
At home, icing the sole of the foot can feel great and can help relieve the immediate soreness. Freeze a bottle filled with water and roll the sole of your foot gently over it for 15-20 minutes. Repeat as necessary.
Stretching exercises are a vital part of medium-longer term management but won’t offer the immediate relief that icing will. But this doesn’t mean you should avoid them! Stretching of the calf is recommended. And sometimes the hamstrings and other parts of the lower limb benefit from stretching.
CLICK HERE FOR YOUR BASIC PLANTAR FASCIITIS CARE

Stubborn plantar fasciitis
Sometimes you can do everything right and still feel as if you’re getting nowhere (I did say it’s a bit of a medical puzzle!) If you’ve been managing your pain properly for 2 months or more but you still see little change, it’s worth looking at Shockwave therapy. Extra Corporeal Shockwave Therapy, to be precise. This is a relatively new form of treatment used for tendinopathy and myofascial conditions.
Shockwaves are high energy soundwaves produced underwater with a high voltage explosion and evaporation – sounds pretty cool right? The theory is that the shockwaves induce neovascularization at the bone-tendon junction and stimulate the release of growth factors to help with cell proliferation. In other words, they improve blood supply and tissue regeneration (1).
While these machines have been around since the 80s, it’s only recently that they’ve been applied to tendinopathy and myofascial issues. The evidence is still growing but is very promising.
1. Dedes, V., Stergioulas, A., Kipreos, G., Dede, A., Mitseas, A. and Panoutsopoulos, G. (2018). Effectiveness and Safety of Shockwave Therapy in Tendinopathies. Materia SocioMedica, 30(2), p.141.
The post Plantar Fasciitis Treatment: Your Options in New Zealand appeared first on MetaMed.
]]>The post Diastasis Recti: What Is It And How Do You Repair It? appeared first on MetaMed.
]]>What is Diastasis Recti?
Diastasis recti is the fancy pants term for abdominal separation. It affects the ‘six-pack muscles' (they are under there!) of your stomach. The anatomical name for your ‘six-pack' is rectus abdominis muscles.
The abdominal muscle separation occurs in both men and women when there is prolonged horizontal stress on the linea alba (line of connective tissue down the middle of your rectus abdominis muscles.
Who Gets Abdominal Separation?
Both women and men can experience a separation of their abdominal muscles. There are a variety of conditions and risk factors that may predispose someone to develop an abdominal separation.

Pregnant Women
Diastasis recti is most commonly seen in pregnant or postpartum women, this is due to the surge of relaxin hormones that help everything to soften. Relaxin allows your ligaments and connective tissue to soften allowing your pelvis to open and accommodate your growing baby and make childbirth easier. It doesn't happen in every pregnancy but this is when we usually see it. It's the common cause of ‘mummy tummy'.
It can happen early in pregnancy or later. It's a good idea to work with a practitioner who commonly works with pregnant women so that they can keep checking if you're starting to develop an abomdinal muscle separation. There are lots of ways you can look after a diastasis to prevent it from getting worse.

Don’t forget the Lads.
Abdominal separation is often missed in men but can contribute to lower back pain. This is why when you come in for back pain we'll look at your whole body to try and work out all the factors you need to address to aid recovery.
We see it lots in farmers and builders. Especially the one with the nice round beer bellies.
Weight gain around the belly area can put extra stress on the abdominal muscles. Pair this with lots of heavy lifting and labor with poor technique over time can lead to separation of the abdominal muscles.
For the men, we often see these many years down the track and it is more challenging to work with, but we can still help. We recommend that if you are in a heavy lifting job that you learn how to use your core properly and take your time with proper lifting technique to prevent it happening in the first place. We recommend seeing a practitioner that understands abdominal separation who can prescribe a specific exercise program that includes core exercises.
For the rest of this article, we'll focus on abdominal separation seen in pregnancy. But guys, get in touch if you think you have this as we can still help you!
How to Detect a Separation
To diagnose diastasis recti a practitioner will feel for a gap between muscles of more than 2cm, further imaging via ultrasound may be used to confirm a diagnosis although not that commonly used.
To test yourself, lie on your back with your knees bent. Supporting your neck with one hand, inhale then exhale and gently lift your neck in an ab crunch like movement. With the other hand, use your fingers to feel in the middle of your abdominal muscles. If your fingers sink in and you feel a gap of more than two fingers, you have a separation.
In more severe cases it may look like doming, bulging, sinking, in the middle of your belly.

What Can Cause It?
It can be hard to tell who exactly is going to get diastasis rectus in pregnancy but there are some things that can make you more likely to develop one.
- Second, third or fourth pregnancy, especially if you had one in a previous pregnancy
- Poor posture of the spine
- Having a weakness of your core control muscles (deep abdominal muscles and pelvic floor)
- Exercising incorrectly during pregnancy
- Lifting excessive loads
What Makes Diastasis Recti Worse?
There is plenty of day to day movements that can make diastasis recti more prominent and prevent healing:
- Sitting up to get out of bed or a chair.
- Getting groceries or strollers in and out of a car.
- Picking up a child.
- Exercises such as plank, sit-ups and squats.
Going back to exercise too quickly post-pregnancy can prevent diastasis repair and can leave you with a ‘pouch’ or ‘mummy tummy' no matter how many crunches you do.
Having an abdominal separation can contribute toward lower back pain, pelvic pain and pelvic floor issues such as incontinence.
If you suspect you have an abdominal separation it's best for you to speak with an experienced practitioner or trainer to learn to modify certain postures, movements and any core exercises or exercise program you do.
Can You Repair Diastasis Recti?
If it gets detected early enough there are definitely ways you can prevent it from getting worse and help restore tension across the separation. This means the gap may still be present but it isn’t so weak anymore. The first six months post-pregnancy is when you have the best chance of improving this.
For pregnant mums, this is where having the right people around you to pick up the signs of diastasis early is important. It may be your midwife, trainer, pilates or yoga teacher, or therapist (Osteo, chiro, physiotherapist).
What Can Help?

Breathing Properly
The main muscle in-charge of breathing sits underneath the ribcage and is called the diaphragm. Normally, the diaphragm pulls down into the belly, making it rise and fall with each breath. During pregnancy the diaphragm is pushed upwards by the growing uterus and baby, preventing you from getting a full, deep breath.
It’s important to retrain your diaphragm to its full function post-partum as it is an essential part of your core. Spend time each day focusing on ‘belly breathing’ by placing your hands on your lower ribs and expanding them outward, without moving the chest. In for 2 seconds, out for 4-6 seconds. Struggling with this? For more information on breathing click here.
Emma Ferris from The Breath Effect has online classes that can help you out too.

Posture
Postural habits formed during pregnancy commonly continue on post-partum. There are two common postures that require correcting to help repair diastasis recti.
- Some women tend to stand with their pelvis pushed forward, forcing stability to come from muscles in your back and glutes.
- Alternatively, do you ‘hang’ from your hips? Pushing your belly forward and over-extending/locking your knees? This increases pressure on the abdominal muscles and can cause increased curvature of the lower spine ‘sway back'.
Bringing awareness to your posture and focusing on ‘postural stacking’ to align your spine. Try not to arch your back or grip any muscle too tight. Imagine a string is pulling you upright from your head, elongating your midline, spine and stretching your ribcage away from your pelvis.
Avoid Constipation
The act of ‘baring down’ when constipated can significantly increase abdominal pressure and increase abdominal separation. Remember to keep your fluids up, consume plenty (25 grams) of fibre each day and exercise. If this doesn’t work, talk to us about herbal remedies that gently get your bowels moving.
Abdominal Supports
Our friends at Pelvic Solutions, women's health physiotherpists recommend wearing abdominal support shorts (similar to spanx) post-partum to help increase awareness of your abdominal muscles and encourage the muscles to come back together. Ideally, you’d wear the shorts for 6 weeks, however, everyone is different and based on your presentation you might need to wear them for longer. While you’re at it, book in with the team at Pelvic Solutions and get your everything checked!

Non-Aggravating Exercises
There are a few easy to implement changes you can make to prevent ‘belly doming’ in day to day life.
- Avoid sit-up type movements, so roll over to your side in bed and use your arms to push yourself up. This reduces intra-abdominal pressure that may prevent diastasis recti repair.
- When lifting, exhale as you lift rather than gripping on tight. Make sure that load isn't too heavy either.
Pelvic Floor Exercises
Kegels! We all know about them. Pelvic floor exercises can help to strengthen the core as well. But, did you know that many women have an overactive pelvic floor? This means kegel exercises aren't appropriate for you. We recommend seeing a women's health physiottherapist to be assessed and taught how do these exercises properly.
Other abdominal core exercises such as bird dog, heel slides and pelvic tilts can help activate the core muscles without increasing intra-abdominal pressure. Not sure about these? We can help!
AVOID: crunches, planks, squats and any other exercise that increases the pressure in your belly.
Once assessed by a practitioner and given the go-ahead you can start reintroducing ab exercises slowly and gradually.
At-home programs
We also love the MUTU at home post-natal exercise programs which are targeted for a new mum with abdominal separation. They're full of great resources around diastasis recti too.

Osteopathy Treatment
Your osteopath can help to diagnose diastasis recti and guide you through the healing stages by advising on the correct breathing habits, postural positions and safe exercises to do. We also love to collaborate with other practitioners and trainers that we know and trust can help you recover and improve your abdominal separation.
As osteopaths we look body wide for compensations in movement patterns and identify any areas that may be contributing to increased pressure on your abdomen. Sometimes you can read all about the issue, but you still need specific and personalised advice to ensure effective healing.
If you are pregnant we also have a great post about what you can do and who you can see at different stages of your pregnancy. Click here to check the post out.

FAQs
Can you fix Diastasis Recti?
Diastasis recti or abdominal muscle separation can be helped.
How do you diagnose Diastasis Recti?
Laying you down, a practitioner will put their fingers over the midline of your stomach (above your belly button). Do a semi sit up. If diastasis recti is present there will be a gap felt greater than one finger wide.
Is Diastasis Recti dangerous?
No. The separation however can get quite large. If a conservative approach doesn’t work (education, postural advice, exercise program and core exercises). This may compromise your ability to stabilise (due to lack of core) and put you at a higher risk of lower back issues. If it is severe you may need a referral to a specialist.
Can Diastasis Recti be painful?
Some people can notice tenderness around the separation particularly around the belly button. More so if there is a hernia present.
What exercises not to do with Diastasis Recti?
You are best to avoid any exercises or movements that cause bulging of the separation or put more stress on the separation. You are best to avoid sit ups or lifting heavy loads.
How do you sleep with Diastasis Recti?
Any position that is comfortable is safe to sleep with an abdominal separation. Just make sure that when you get up from laying to sitting don’t sit straight up. Roll onto your side and use your hands to push yourself up.
The post Diastasis Recti: What Is It And How Do You Repair It? appeared first on MetaMed.
]]>The post Chronic Pain and the Brain appeared first on MetaMed.
]]>The physiological phenomenon of pain is so complex that even leading researchers cannot claim to comprehend it entirely. But our body of knowledge is growing and we all have the ability to understand the basic pain biology. Education, knowledge and understanding will reduce the threat associated with pain and will change how we think about it. This has to be the first step to pain management. First, we may need to reconsider what we already know …
What are your beliefs around pain?
· Do you think all pain, no matter how big or small, equates to some amount of bodily damage?
· Do you believe that increased pain equals a worse injury?
· Do you think pain always has a physical cause?
If you answered yes to one or more of these, you join the majority of people (including some health professionals) who have misconceptions regarding pain.
Breaking down pain
Let’s take it back to basics. We can break down types of pain into Acute and Chronic.
Acute pain: Just rolled your ankle running down a trail, or caught your arm on a hot pan? That’s acute pain. It tells us that we’ve just done something potentially harmful, or may have caused some damage to our bodies. This kind of pain is really useful! It forces a reaction to move away from the hot pan, or to stop running down that trail so we avoid any more damage and give ourselves a chance to heal! The pain goes away over a few days or weeks because there’s no more threat to the body, and the tissues have a chance to heal.
Chronic Pain: Technically we define this as a pain which has persisted for 3-6 months or more, but essentially, we recognize it as pain which persists longer than the necessary tissue healing time. We know that neurons (nerve cells) in the brain adapt and become much more efficient at carrying danger messages and therefore much more efficient at producing pain. We also know these neurons lose their ability to be specific. This means the pain is more easily triggered, but less informative. If you have been diagnosed with chronic pain you’re not alone: 20% of people worldwide are estimated to be affected.
So, what causes the shift from acute to chronic pain in some people?
There’s no definitive answer to this, but the short version is: almost anything can affect pain. It’s complex and multi-factorial. Nerves send danger messages to the brain the brain then checks with the sensory centre, emotional centre, motor centre, memory centre and many more before making a split-second decision on whether to give an output of pain – and how much. The brain then continues to update its assessment of the situation. Ever had an injury where you looked down and realised your bleeding? And then like flicking a switch the pain starts? That’s because the brain relies on context!

What can we do About it?
Researchers and health professionals are re-shaping the way we manage chronic pain. We now know that education, knowledge and understanding can physically change what’s going on in our brain, literally re-shaping the connections between these neurons!
Your practitioner can help with this! Our role is not just hands-on therapy, but to educate as well. Treatments which combine manual therapy with education, and specific movement-based strategies have been shown to be much more effective.
Essentially, we want to help change the way you think about chronic pain. We can recommend literature and other resources that are designed specifically for people with chronic pain, and develop a plan which includes techniques to decrease neurological sensitization.
References:
Moseley and Butler: EP supercharged
Monica Noy: www.monicanoy.com
The post Chronic Pain and the Brain appeared first on MetaMed.
]]>The post Tendinopathy Treatment – Overuse injuries and pain reduction appeared first on MetaMed.
]]>There are two common types of tendon injuries, tears/ruptures and overuse injuries known as tendinopathy. Tendinopathy is an umbrella term that encompasses a variety of reasons for tendon irritation. Research is being carried out on the best approach to treating tendinopathies, with new and improved treatment criteria being published all the time.
What is tendinopathy?
Tendinopathy (tendon injuries) occur when the tendon (the fibrous connective tissue that attaches your muscles to your bones) is unable to maintain the load being placed on it. It was originally believed that this caused inflammation. But we now know this isn’t the case. Instead, the tendon swells with oedema (clear fluid) and the nice, tidy, uniform collagen fibres in the tendon become ‘irregular’ causing failed attempts at healing.
Tendons are tough cookies. They can maintain tension for long periods and require much less oxygen that muscles. However, this also means they are frustratingly slow to heal, which means those with tendinopathy get frustrated. Why are they STILL not better?
What causes it?
The main risk factors are
1. Sudden change in activity, particularly those that require a load to be placed on the tendon (running, jumping, walking).
2. Compression on the tendon – think: pressure on your Achilles from shoes or falling on your knee and impacting your patella tendon.
3. Predisposition due to systemic factors such as high cholesterol, smoking, age.
4. Predisposition due to biomechanics such as poor muscle capacity/contraction or misalignment.
Symptoms
Symptoms will vary depending on the location, but in general, the tendon will be tender to touch, for example, an aggravated Achilles tendon will be painful when pinched, this is a sign of injury or irritation. Pain levels will increase with exercise, repetitive movements or increased use/load.

Types of tendinopathy
Stage 1 – Reactive: sudden increase in load or direct impact can cause the tendon to swell, thicken and become stiff – a natural protective response to reduce the stress being placed on the tendon. This is a relatively short-term stage and the best time to act as the structure of the tendon is intact and can return to normal. However, people commonly try to ‘push through the pain’ during this stage and don’t adapt their activity enough to allow sufficient healing. So we move on to stage 2.
Stage 2 – Dysrepair: occurs when the load is not decreased and the tendon has not returned to normal. The structure of the tendon begins to change, collagen separate and becomes disorganised, a sign of failed healing. However, during this stage it is still possible to heal the tendon and return to full strength
Stage 3 – Degenerative: The tendon has had multiple failed healing attempts and changes to the structure are irreversible. The tendon will be thickened and may have nodular, hard sections. This usually occurs in those that have continued to stress/load the tendon and older individuals with on-going tendon issues. The tendon is stiff and weak, predisposing to rupture as it has less capacity to adapt to the loads placed upon it.
Commonly affected areas
Shoulder
Rotator cuff and biceps tendons commonly cause pain in the front and side of the shoulder. The rotator cuff is made up of four different muscles, but one muscle is affected more frequently than others – the supraspinatus muscle. Tendinopathy of the supraspinatus muscle will cause pain and weakness when lifting your arm overhead, increased pain when sleeping and pain may travel down to your forearm/wrist/top of the hand. The biceps muscle often follows on from supraspinatus tendinopathy or if there is damage to the rotator cuff muscles. However, it can happen in isolation if there is repetitive heavy lifting. As such, the pain will intensify when lifting heavy objects.
In both cases, there may be an increase in popping and clicking of the shoulder joint due to increased fluid and swelling in the area.
Elbow
Technically known as medial epicondylitis (golfers elbow) or lateral epicondylitis (tennis elbow). It involves the tendons from your forearm muscles and where they attach at the inner or outer elbow. Despite the name, it is infrequently caused by golf or tennis! Commonly seen in sports/jobs that involve repetitive twisting of the wrist, computer use, vibration or heavy lifting. Symptoms include tenderness over the tendon, reduced grip strength, pain may radiate into the wrist and hand, painful resisted wrist extension/flexion.
Wrist
A common wrist tendon issue is De Quervain’s. De Quervain’s tenosynovitis is a little different from the other examples here as it involves the tendons of two small muscles in the forearm; the tendons are housed in a sheath that can get inflamed, preventing smooth gliding of the tendons as the muscles contract or the wrist bends. However, the cause is the same; repetitive use of the thumb with a sideways movement of the wrist. Overloading these tendons causes them to swell, reducing the space in the sheath, leading to pain and stiffness.
Hip
The gluteus muscles are a group of three muscles that make up your buttocks. Gluteal tendinopathy causes pain in the side of the hip and is common in runners and inactive people. Pain here can be caused and aggravated by sleeping on your side, sitting with legs crossed and running with a gait that crosses the midline on contact. Gluteal tendinopathy pain will increase slowly over time and will be accompanied by stiffness, however, range-of-motion should not be decreased.
Knee
The patellar tendon attaches your quadriceps to your knee cap and down to your shin bone. Patellar tendinopathy usually occurs in younger athletes (15-30yrs) who repetitively load the tendon through jumping, suddenly stopping or changing of direction. Sports such as basketball, tennis and football commonly cause patellar tendinopathy. The pain will be felt in the front of the knee, commonly below the kneecap.
Ankle – Achilles
Achilles tendinopathy can happen in two places, 1) where the tendon joins to the ankle, or 2) where the tendon turns to muscle (called the musculotendinous junction or MTJ). Achilles tendinopathy is hallmarked with morning pain that slowly gets better the more you walk around. This is because the tendon has to perform to full range of motion with basic movements such as standing and walking, stretching and irritating the tissue. Swelling will be minimal – however the affected tendon will be thicker in diameter and may have a painful nodule compared to the unaffected side.
Tendinopathy treatment
While the location of tendon injuries is variable, the approach to treatment is the same:
- Offload: Give the tendon a period of rest. Spend time stretching other muscles around it, but not the affected muscle/tendon. For example; rotator cuff tendinopathy could involve stretching the chest muscles (pec major/minor) and back muscles (latissimus dorsi) to encourage optimum shoulder positioning and movement.
- Gradually load: Eccentric exercises have proven results in helping the tendon to remodel and increase tolerance and strength. Eccentric exercises involve the muscle lengthening while contracting – eg: bicep curl in reverse. Progressing to weight/multidirectional/fast-twitch muscle fibre training. Your practitioner can help guide you with exercises for your specific injury.
- Movement/biomechanics: Changing the way we move works on the root cause of the problem and can help prevent recurrent injuries. For example, a runner's gait can have a big impact on how much the Achilles tendon is loaded.
- Manual therapy: Most importantly, an osteopath/physio can help guide you in the above approach to treatment. They can also provide you with some relief from pain and promote tissue healing through massage techniques and acupuncture – helping you to achieve your goals and get back to doing what you love.
- Other: Shock-wave therapy, laser therapy, platelet-rich plasma or corticosteroid injections – these modalities are all used in the treatment of tendinopathy with varying results. Your practitioner can explain them all and help refer if needed.

Summary
While we don’t know everything about tendinopathy treatments, here are some undeniable truths that every patient needs to keep in mind:
· Rest alone is not the answer. It may settle and reduce the pain in the interim but returning to activity is often painful again. This is because rest does nothing to increase tendon load tolerance.
· Tendinopathy is not considered to have a classic inflammation response. That being said, research has found that ibuprofen is helpful in the early stages to assist in tissue repair.
· Those with a predisposition to tendinopathy may find that even a subtle change will cause a flare-up, which will then take a long time to heal.
· Reducing the load initially to settle the pain is important. A short-term reduction in the aggravating movement/compression is required.
· Research has found that the best treatment for tendinopathy is exercise. Sorry people, but if you want to get better you will need to do the exercises you practitioner gives you. A lot. For longer than a week. Tendons need to be loaded slowly and progressively to increase their tolerance to load. In most cases, a tendon will continue to be painful and repetitively flare up if this crucial stage is missed.
· Similarly, tendinopathies rarely heal with passive treatments alone. By this I mean, just getting osteopathic treatments/injections/shockwave therapy/acupuncture will not fix your issue. In fact, multiple injections have been found to disrupt the healing process!
· Everyone is different. Everyone moves differently, places different strains on their body, has different predispositions, tolerates pain differently. Therefore, exercise needs to be individualised.
· As per our blog post on imaging: the diagnosis on imaging is not equal to the pain you feel. Some people have tears, tendinopathy, calcifications and are asymptomatic. For this reason, treatment focuses on your improving pain levels and function rather than sending you off for repetitive imaging to check on tissue healing.
· Most importantly, remember – Tendons heal slowly. They respond very slowly to exercise and you need to have patience. It may be tempting to resort to the ‘quick fix’ of an injection or surgery, but in reality, there is no easy way out. Put the time and effort in and you will feel better eventually.
References
(J. L. Cook, Rio, Purdam, & Docking, 2016; J. Cook & Purdam, 2012; Coombes, Bisset, & Vicenzino, 2010)
Cook, J. L., Rio, E., Purdam, C. R., & Docking, S. I. (2016). Revisiting the continuum model of tendon pathology: what is its merit in clinical practice and research? British Journal of Sports Medicine, 50(19), 1187–1191. https://doi.org/10.1136/bjsports-2015-095422
Cook, J., & Purdam, C. (2012). Is compressive load a factor in the development of tendinopathy? British Journal of Sports Medicine, 46(3), 163–168. https://doi.org/10.1136/bjsports-2011-090414
Coombes, B. K., Bisset, L., & Vicenzino, B. (2010). Efficacy and safety of corticosteroid injections and other injections for management of tendinopathy : a systematic review of randomised controlled trials. The Lancet, 376(9754), 1751–1767. https://doi.org/10.1016/S0140-6736(10)61160-9
Gattie, E., Cleland, J., & Snodgrass, S. (2017). The Effectiveness of Trigger Point Dry Needling for Musculoskeletal Conditions by Physical Therapists: A Systematic Review and Meta-analysis. Journal Of Orthopaedic & Sports Physical Therapy, 47(3), 133-149. doi: 10.2519/jospt.2017.7096
Liao, C., Xie, G., Tsauo, J., Chen, H., & Liou, T. (2018). Efficacy of extracorporeal shock wave therapy for knee tendinopathies and other soft tissue disorders: a meta-analysis of randomized controlled trials. BMC Musculoskeletal Disorders, 19(1). doi: 10.1186/s12891-018-2204-6
Miller, L., Parrish, W., Roides, B., & Bhattacharyya, S. (2017). Efficacy of platelet-rich plasma injections for symptomatic tendinopathy: Systematic review and meta-analysis of randomised injection-controlled trials. BMJ Open Sport & Exercise Medicine, 3(1), e000237. doi: 10.1136/bmjsem-2017-000237
Tumilty, S., Munn, J., McDonough, S., Hurley, D., Basford, J., & Baxter, G. (2010). Low Level Laser Treatment of Tendinopathy: A Systematic Review with Meta-analysis. Photomedicine And Laser Surgery, 28(1), 3-16. doi: 10.1089/pho.2008.2470
The post Tendinopathy Treatment – Overuse injuries and pain reduction appeared first on MetaMed.
]]>The post Why Do I Need Treatment if I’m Not in Pain? appeared first on MetaMed.
]]>People often think to only seek treatment or therapy when they are in pain.
Most of us feel niggles and strains, and we recover. Other times we feel them and we hope they'll get better on their own… but then they keep getting worse, and interfere with your day, work or life in general. That's a real pain!
You might take the odd pain killer, because that's easier…
It works for a while…
But then they stop working!
By the time you are in pain, your body has already reached crisis point. That's why it's screaming out to you to do something.
Our Body Is Capable, Until It's Not
Our body does an amazing job at compensating, meaning it can hold things together and keep working even when things aren't quite right, but if you stress it too much physically, emotionally, mentally it can only handle so much. Everyone has different thresholds, some greater than others.
So often we don't see people until they're in pain, but the issue may have been brewing for many days, weeks or months just waiting to rear it's head.
Our initial focus is to get you out of pain. This is when you can think clearer, move freer and get back to doing the things you love.
The Vicious Cycle
So many people feel great after two or three treatments then decide they don't need anymore. We love that feeling too, but unfortunately, we see the following pattern reoccur.
- You come in for pain…
- You feel better after a couple of treatments…
- You decide you don't need any more treatments…
- Then a few weeks later your pain starts to slowly creep back in…
- It gets intolerable…
- You feel like you're never going to get better…
When you get into the thought that you're never going to get better, that's not a nice place to be.
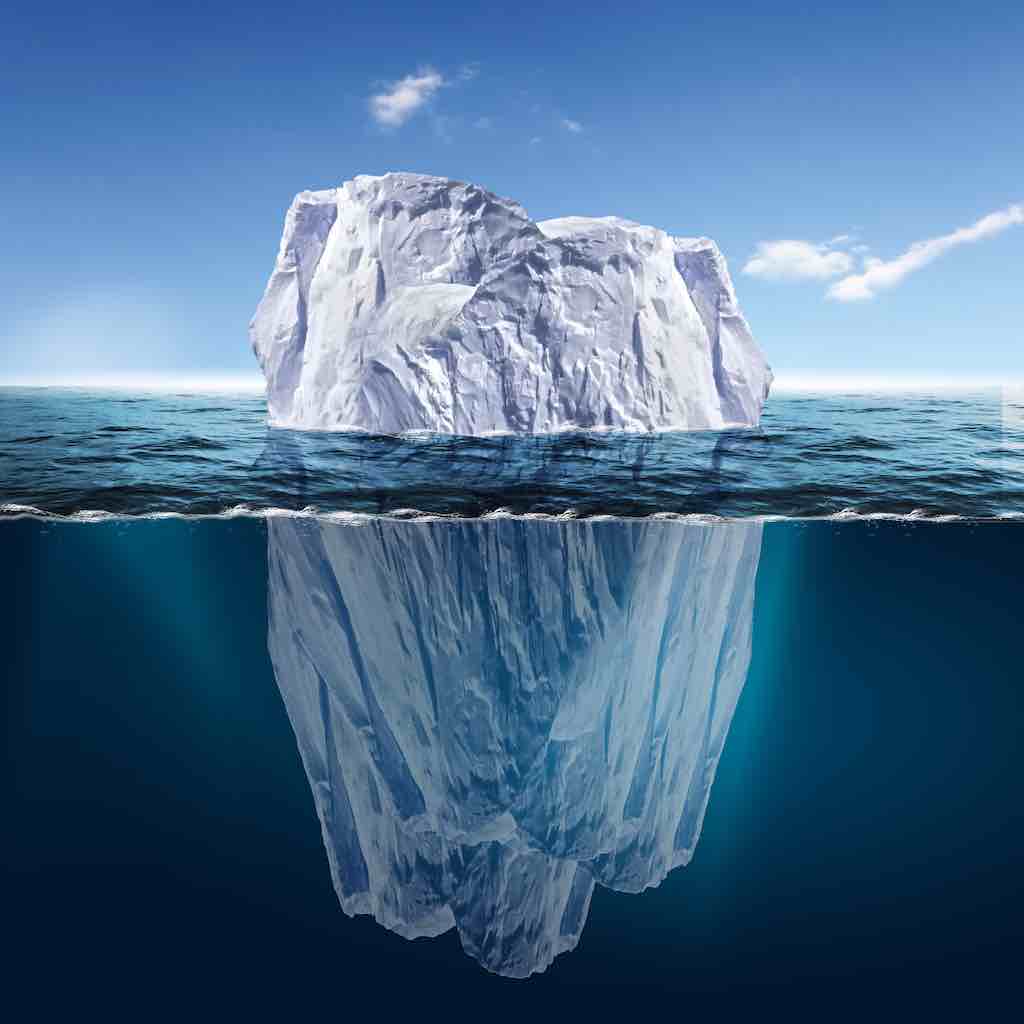
Your Body Like an Iceberg
In the above video, Dr. Auria Young our holistic chiropractor discusses how your body is like an iceberg. This is how we can best explain why your pain comes back when you stop treatment.
Your pain is everything you see above the water. Over time you have physical therapy and chip away at the painful areas. You feel great once you can no longer see the iceberg.
But look at how much is brewing under the surface, waiting to build up again.
So when you get to the water level, you're not in pain. The reason we recommend maintenance treatment is to keep chipping away at what is below the surface. To get to the root of the issues so that your problems take longer to arise again.
Maintenance Treatment
You've probably heard this term over and over again. And the analogy of the car. If not, here it is again.
Think about how you look after your car, taking it for regular WOFs and servicing (hopefully) so it keeps running to get you from A to B. If something doesn't sound right, or a light flickers on your dashboard, you go get it checked out. Because you need your car to keep working for you!
If you ignore the sounds and the lights, it may keep going for a little while. However, one issue may have a knock-on effect to another area of your car. It keeps going… until it can't anymore.
If you look after your car. Look after your body as your vehicle, to run efficiently, get you from A to B and make life easier!
If you don't look after your car, you may have to rethink things a little. Do you not look after your car, just like your body?
Do I Have to Keep Coming in Forever?
People come in depending on how long their body can hold a treatment. Various factors are involved and is entirely different for everyone.
Things that can impact:
- Stress – mental and physical
- Lifestyle
- Diet
- Environment
We aim to have you independent of treatment as much as possible. This may mean you need to make changes in lifestyle and stress situations that you are able to change. It may also mean you need to engage in stretches or rehab exercises, start a new activity to support your body.
People can come in from anywhere between every three weeks to 3-4-6 months!
The best part is they come in feeling great, become more aware of their body holding tension and reduce the rate of injury, or recover much faster from injury.
Self-Care
Allowing yourself to get treated is a great self-care tool. It keeps your mind-body balance, keeps you going and doing what you love.
The post Why Do I Need Treatment if I’m Not in Pain? appeared first on MetaMed.
]]>The post How To Use Massage Balls appeared first on MetaMed.
]]>
Tight and achey muscles but can't get in to have a massage or treatment?
Massage and hands-on work is a great way to relieve muscle tension, but sometimes it can be hard to find the time.
Thankfully there's an array of self-care tools including massage balls out there to help you. But you may not be so sure how to use them.
Benefits of massage balls
- Quick and easy massage tool
- Treat yourself between massages or treatment
- Improve blood flow
- Improve muscle recovery
- You can control the pressure
Smooth or Spikey?
Laura Randall our Osteopath will take you through the benefits of each type of massage ball.
Benefits of the smooth ball:
These myofascial balls are great to get into more sensitive areas, or if you're just starting out with massage balls.
Benefits of the Spikey Ball:
The spikey ball is a bit harder with little nobbles to get into all the nooks and crannies. If you need some deeper work a spikey ball can be great to get deeper into your muscles.
Quick and easy tips to relieve tension

- Roll your feet for 5 minutes to relieve tired and achey feet
- Lay on your back with the ball under a trigger point, lay there for a couple of minutes until the trigger point releases
- Place the ball under your neck as you lay over it
- Roll the ball over your muscles to improve blood flow
When Not to Use Massage Balls
There are times when it's not appropriate to use massage balls. If you're unsure seek professional advice.
- Fresh injury
- Broken skin
- Too painful or uncomfortable
- Makes your symptoms worse
Dr. Nick’s Spiky Break-Down FAQ
What do Massage/Spiky Balls do?
The key concept behind the use of spiky and other massage balls is that the application of pressure to an area of the body can be useful in order to obtain various health benefits. This parallels the effects of deep tissue massage techniques when you see a manual therapist such as an osteopath, chiropractor or massage therapist. Therefore, any object, being spherical in nature or otherwise, can be used to apply pressure and achieve the desired result. Just as the bear scratches its back using the bark of a tree, so too can we use a golf/tennis/lacrosse ball, or even a foam roller for that matter, to massage our muscles and improve tissue tensions.
As I said, the object need not be a ball at all. There have been several occasions when I’ve been crippled by pain while travelling abroad and I’ve resorted to digging into the pantry to pick out two cans of tinned beans just to roll out my lower back – repeatedly falling on your neck when trampolining isn’t recommended! As long as those cans don’t open while you’re on top of them you’re good to go! With that said, it is probably less often when you find yourself in a position where you don’t have access to at least a tennis ball at the bare minimum.
What to Look for in a Massage/Spiky Ball?
The benefit of using a spherical object like a ball is that you can roll along or across the length of your muscles, simulating the action of having a massage. If we’re talking specifically of massage balls, there are four main differentiating factors: size, density, friction component (how grippy the ball is), and whether or not the ball is spiky. The first three factors are by far the most important. A golf ball is small, extremely firm and generally has a low friction component. A similar-sized ball is a squash ball which is small, less firm but very grippy. Size and density are fairly self-explanatory, a small ball is easier to work into tight spaces like between the ribs or into the small muscles of the foot, and the density determines how much pressure you can exert. Similarly, a large ball covers more surface area and can be better suited to penetrating deeper into the larger muscle groups – much the same as a foam roller is generally better suited to releasing the larger muscle groups. The friction component can be important so that the ball doesn’t slide out from under you if you’re lying on it or leaning against it on a wall which can be quite important too. There are various ‘points’ of view in relation to how important the spikes on spiky balls are. It is theorised that they elicit a greater stimulation of local blood flow in the capillaries, but there appears to be little if any evidence to back this up.
Personally my favourite all-round self release tool is a lacrosse ball. For the enticingly low cost of $5-10 this ball has all of the qualities I like in a massage ball. It’s very firm but not unyielding, is small enough to be useful to get into smaller knots and muscle groups but still large enough to release deep tensions in the quads and glutes, it also has a high friction component, meaning you can use a lacrosse ball on a slippery wooden door or flooring and it’s unlikely to slide out from under you. A tennis ball is a close runner-up because of its ubiquitous nature and having similar size to a lacrosse ball, but rubber cricket balls and baseballs work too. I also really like golf or squash balls for releasing the small muscles of the foot.
Some Tips for Application
- Putting a massage ball in a sock is a great way to target difficult-to-reach back muscles when leaning against a wall. Hold the end of the sock in your hand and hang the ball down to the desired area of your back or shoulder.
- Taping two tennis/lacrosse balls together to form a ‘peanut’ is a great way to apply even pressure to the muscles on either side of your spine while still leaving a divot for your spine to notch into. This is a much stronger way to release your spinal muscles than using a foam roller and has the significant benefit of not being deflected by the shoulder blades. Best results are achieved by lying on the peanut and using your body weight to apply pressure.
- For some people, it can be a daunting process to workout [sic] exactly what and where to apply pressure to. My advice is always to take an open-minded approach. Use the massage ball as a way of exploring and discovering your body in a new way. Really try to feel the tensions in your body and use that new information to guide your self-release exercises. Personally, I’ve always seen it as a form of masochistic meditation like Vipassana – you have the ability to stare down your pain and master it. All the while, the degree of pressure and pain is totally up to you, so try to enjoy!
The post How To Use Massage Balls appeared first on MetaMed.
]]>The post Prevent Knee Surgery appeared first on MetaMed.
]]>We find that many people have been told, you’ll need an operation on your knee for it to improve, or ‘you have arthritis’ and there’s nothing we can do, ‘you need to get a knee replacement.'
In some cases yes surgery is the best option especially if your knee is causing you a lot of discomfort, instability and you’re unable to normal daily activities.
However, for those who have been told this before they’ve even tried conservative (non-invasive) treatment – hands-on treatment, manual therapy, exercise
Why is Your Body in Pain?
Much of the time if there
The pain can often be due to muscular tension (typically a dull ache), and yes you may have some changes in the structure of your
Treatment is Not Just Pain Relief
But pain relief is not the only benefit. If you are heading down the road of surgery, this means you’re going to have to rehab to get the most out of it!
Treatment is also an opportunity to help you slowly learn corrective exercises. Often pain can cause muscles to turn off, and it’s difficult to learn how to use them again!

Prehab
By easing discomfort your body is more willing to engage muscles and strengthen them. We call this time prehab. It’s doing the work to get you in the best shape in prep for surgery so that you have optimal outcomes and get the most out of surgery,
Exercises to Get You Started
DOWNLOAD our basic knee exercises. *Please note that you may have some difficulty engaging these muscles if you have a chronic knee injury. This is where we can help with treatment. To help stimulate your muscles to make it easier to exercise them.
Benefits of Treatment Before Surgery
And, sometimes we find that people who so urgently needed surgery, actually don’t! They can reduce their pain killers, return to some level of activity and post-pone surgery for months or years.
So if you’ve been told you have a degenereative knee. Lets help either get you in shape for surgery or even prevent it needing to happen in the first place!
How Does Arthritis of the Knee Develop?
The progression towards arthritis is usually because of a previous trauma or injury causing a change in mechanics and load to your joint. In your knee it could be:
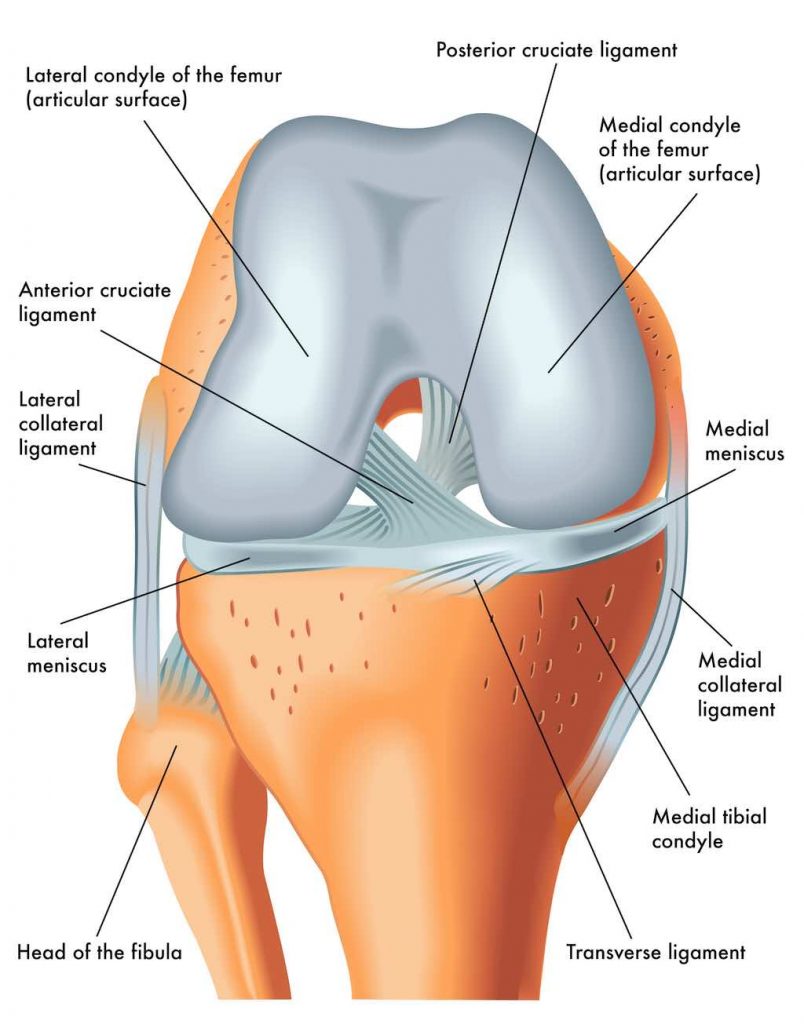
- Sprain knee – injury to the medial or lateral collateral ligaments
- Cartilage issue – meniscus tag or tear
- Internal ligament damage – the anterior cruciate ligament or posterior cruciate ligament

Address the Issue
As always, it’s important to address the underlying reasons that may have led to your condition in the first place: Existing weakness, biomechanical issues which need correcting etc…
Don’t get us wrong, we’re not against surgery at all. It is amazing what it can do. But don’t use it as your only ‘fix’.
The post Prevent Knee Surgery appeared first on MetaMed.
]]>