The post Chiropractic Care In Pregnancy appeared first on MetaMed.
]]>Why is Pain Common?
The female body is amazing at adapting to the growing baby. During pregnancy, a hormone called relaxin allows the ligaments in the body and around the pelvis to relax and soften. This allows the pelvis to expand while in labour and accommodate the growing baby. This is a very important process the body goes through and can facilitate more movement through the joints. This increase in movement with the added stress and pressure from a growing baby can lead to inflammation and the sensations of pain.
The most common places pregnant women experience discomfort is at the pubic symphysis (SPD) and the sacroiliac joints in the pelvis. The result spinal, low back pain and pelvic pain.
How to Prevent Pain in Pregnancy
The first trimester is not a common time to experience discomfort but is a great time to get into a good pre-baby care routine. This is the perfect time to prepare by choosing stability and endurance exercises to get the deep core, pelvic floor and pelvic stability muscles working. This helps minimise the stress placed through the spine and pelvis in pregnancy. It will also help make labour easier and help the pregnant mother's body spring back into good shape postpartum.
The recommended exercises will be slightly different to a “normal” routine so it is important to find a professional who can guide you through the different exercises at each stage of your pregnancy. A specialised personal trainer or a pregnancy chiropractor with pre and postnatal management training is essential.
Chiropractic care can start through any trimester and we recommend starting by the end of your first trimester as a preventative approach. It's also a good part of your pre-baby body care routine. It is far better to get into a good routine rather than to wait. But for some, this isn’t an option so chiropractic care can be started as a pain management approach whenever possible.
Benefits of Chiropractic Care During pregnancy
There are many benefits. Chiropractic treatment can make pregnancy more enjoyable, labour easier, and recovery quicker.
Your chiropractor will ensure that your body is well aligned, your muscles are working well, and your posture is balanced. This helps to restore and maintain the proper function of the body.
The added bonus of a well-aligned posture is that the “internal” will also be well aligned. This is not a common topic of discussion but any external misalignment can result in an internal misalignment. Torsion through the pelvis can translate to the womb and cause a torsion through the womb. This can alter the available space and the positions the foetus can adopt. The result can often be a more painful, prolonged labour and uneven pressure distribution through the pelvis, spine and hips.
Treatment is safe and can be done through each trimester of pregnancy. Specialised pregnancy techniques will vary for each stage and can be catered to your needs.
The chiropractic adjustments where you hear the ‘cracking’ are only performed after the first 13 weeks of pregnancy. It is perfectly safe with no known contraindications. We don't recommend doing this on your own. It is a technique that should only be performed by a trained professional.
A good health care and exercise routine will help through labour and will aid postnatal recovery.
What if the Baby is Breech?
If the baby is in a breech position, chiropractic care and other positional techniques have been shown to help the baby turn on its own shortly after treatment. Chiropractors don’t perform external cephalic version (ECV). This is only performed by specialized doctors but there are other techniques that chiropractors can use that have been shown to be safe and effective.
Postnatal Care
Birth is a traumatic process on the body, whether it was a natural birth, c-section or induced labour. The birth process will have major effects on the muscles, skeletal system and the soft tissues in the body. Care after birth can help aid a speedy recovery and get you back to moving well.
Chiropractic care is also safe for the treatment of babies and it is always recommended to get a newborn checked. Ask your paediatric trained pregnancy chiropractor for more details on the benefits.
The post Chiropractic Care In Pregnancy appeared first on MetaMed.
]]>The post How To Prevent Muscle Cramp appeared first on MetaMed.
]]>Cramp develops when you have an involuntary over contraction or sustained muscle contraction. Either way, it's a pain in your life that you don't need.
What Do Normal Muscles Do?
Normally muscles are constantly contracting and relaxing (shortening and lengthening). Signals from nerves into the muscle tell it to contract, and signals feeding back to our spine and brain then send signals back out to the muscle to relax. The constant process keeps the muscle at a nice resting tone, not too tight and not too loose. This is what we call resting muscle tone.
Cramp Is Like A Short Circuit
You could see a cramp as a short circuit in the system where nerves signaling to the muscle are telling it to contract more and more, but the feedback isn't there for messages to be sent back to the spine and brain to send new signals out to tell the muscle to relax.

What Does Cramp Feel Like?
Cramp is different from a tight and sore muscle. It's usually a very strong contraction. It commonly occurs in the calf, but any muscle can be affected, fingers, toes, shoulder, quads, etc…
You may feel your muscles harden, toes curl and then you feel like you’ve been punched in the muscle for the rest of the day. A severe cramp can cause involuntary movement of fingers and toes or make you rigid with the pain.
What Causes Cramp?
- Poor muscle conditioning – lack of strength or appropriate training
- Overworked muscles including overtraining
- Lack of stretching – yes, it really does help
- Magnesium deficiency
- Dehydration

5 Tips To Help Cramp
- Drink plenty of water. Add electrolytes if sweating a lot. Amounts of fluid consumption will vary on your age, sex and activity levels. If your pee is dark yellow, you need to drink more.
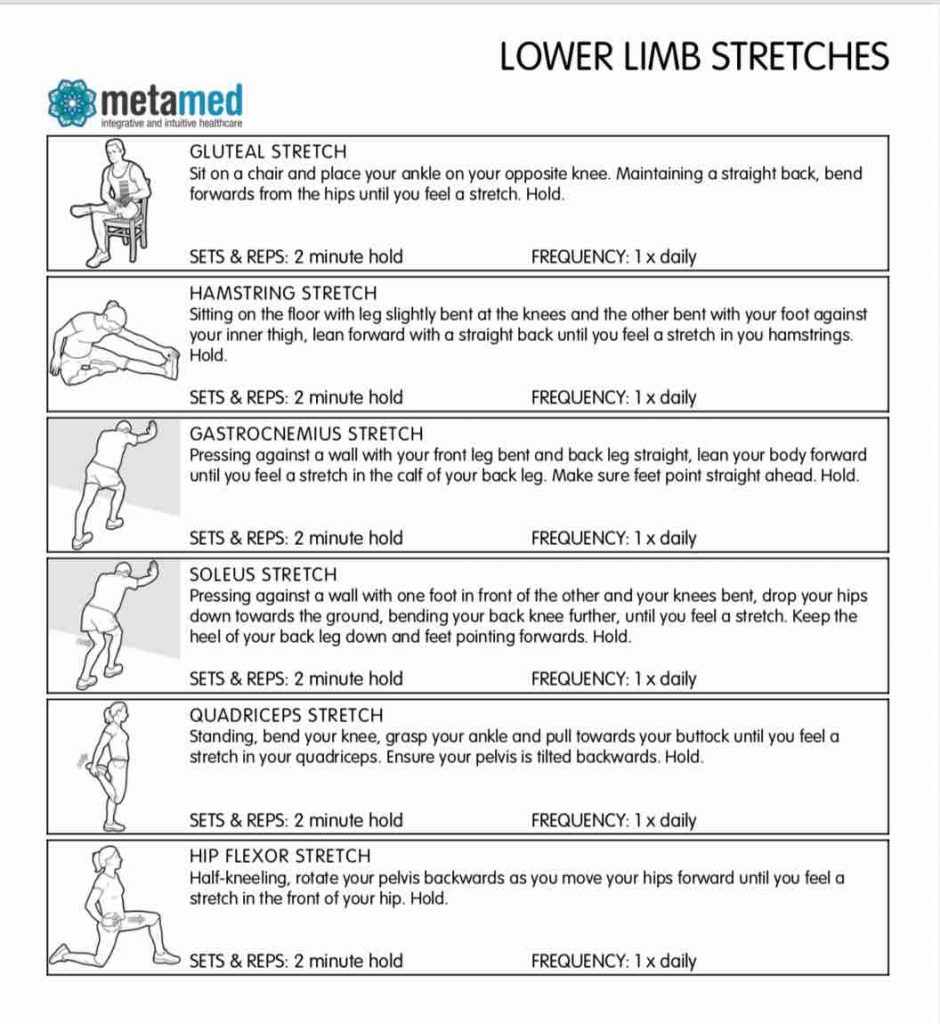
- Hold your stretches for 2 minutes. Set your timer, it's a long time. See the link for our lower limb stretches below.
- Massage yourself: use your hands, spikey balls or foam rollers. Or we think it's much nicer to get someone else to do it for you.
- Magnesium supplementation. A general dose is 300 mg per day (great to take at night to help sleep and ease cramps that get you when you sleep. In pregnancy, the risk of cramp can be higher and dose can be increased to 350-360 mg per day. For active males, a dose of up to 420 mg can be taken. Have a read of our Magnesium blog about the different types to ensure you get an absorbable form right for you.
- Dry needling. If you've tried all of the above and still experiencing cramp you still have options. We love using dry needling to help ‘reset' muscle tone and nerve input. It's highly effective for relieving muscle tension, especially cramping.
If you're suffering from cramp don't keep waiting for it to get better on its own. Seek help with our holistic practitioners. We have osteopaths at MetaMed Wanaka and osteopaths and chiropractors at MetaMed Queenstown experienced with treating cramp.
The post How To Prevent Muscle Cramp appeared first on MetaMed.
]]>The post Tendinopathy Treatment – Overuse injuries and pain reduction appeared first on MetaMed.
]]>There are two common types of tendon injuries, tears/ruptures and overuse injuries known as tendinopathy. Tendinopathy is an umbrella term that encompasses a variety of reasons for tendon irritation. Research is being carried out on the best approach to treating tendinopathies, with new and improved treatment criteria being published all the time.
What is tendinopathy?
Tendinopathy (tendon injuries) occur when the tendon (the fibrous connective tissue that attaches your muscles to your bones) is unable to maintain the load being placed on it. It was originally believed that this caused inflammation. But we now know this isn’t the case. Instead, the tendon swells with oedema (clear fluid) and the nice, tidy, uniform collagen fibres in the tendon become ‘irregular’ causing failed attempts at healing.
Tendons are tough cookies. They can maintain tension for long periods and require much less oxygen that muscles. However, this also means they are frustratingly slow to heal, which means those with tendinopathy get frustrated. Why are they STILL not better?
What causes it?
The main risk factors are
1. Sudden change in activity, particularly those that require a load to be placed on the tendon (running, jumping, walking).
2. Compression on the tendon – think: pressure on your Achilles from shoes or falling on your knee and impacting your patella tendon.
3. Predisposition due to systemic factors such as high cholesterol, smoking, age.
4. Predisposition due to biomechanics such as poor muscle capacity/contraction or misalignment.
Symptoms
Symptoms will vary depending on the location, but in general, the tendon will be tender to touch, for example, an aggravated Achilles tendon will be painful when pinched, this is a sign of injury or irritation. Pain levels will increase with exercise, repetitive movements or increased use/load.

Types of tendinopathy
Stage 1 – Reactive: sudden increase in load or direct impact can cause the tendon to swell, thicken and become stiff – a natural protective response to reduce the stress being placed on the tendon. This is a relatively short-term stage and the best time to act as the structure of the tendon is intact and can return to normal. However, people commonly try to ‘push through the pain’ during this stage and don’t adapt their activity enough to allow sufficient healing. So we move on to stage 2.
Stage 2 – Dysrepair: occurs when the load is not decreased and the tendon has not returned to normal. The structure of the tendon begins to change, collagen separate and becomes disorganised, a sign of failed healing. However, during this stage it is still possible to heal the tendon and return to full strength
Stage 3 – Degenerative: The tendon has had multiple failed healing attempts and changes to the structure are irreversible. The tendon will be thickened and may have nodular, hard sections. This usually occurs in those that have continued to stress/load the tendon and older individuals with on-going tendon issues. The tendon is stiff and weak, predisposing to rupture as it has less capacity to adapt to the loads placed upon it.
Commonly affected areas
Shoulder
Rotator cuff and biceps tendons commonly cause pain in the front and side of the shoulder. The rotator cuff is made up of four different muscles, but one muscle is affected more frequently than others – the supraspinatus muscle. Tendinopathy of the supraspinatus muscle will cause pain and weakness when lifting your arm overhead, increased pain when sleeping and pain may travel down to your forearm/wrist/top of the hand. The biceps muscle often follows on from supraspinatus tendinopathy or if there is damage to the rotator cuff muscles. However, it can happen in isolation if there is repetitive heavy lifting. As such, the pain will intensify when lifting heavy objects.
In both cases, there may be an increase in popping and clicking of the shoulder joint due to increased fluid and swelling in the area.
Elbow
Technically known as medial epicondylitis (golfers elbow) or lateral epicondylitis (tennis elbow). It involves the tendons from your forearm muscles and where they attach at the inner or outer elbow. Despite the name, it is infrequently caused by golf or tennis! Commonly seen in sports/jobs that involve repetitive twisting of the wrist, computer use, vibration or heavy lifting. Symptoms include tenderness over the tendon, reduced grip strength, pain may radiate into the wrist and hand, painful resisted wrist extension/flexion.
Wrist
A common wrist tendon issue is De Quervain’s. De Quervain’s tenosynovitis is a little different from the other examples here as it involves the tendons of two small muscles in the forearm; the tendons are housed in a sheath that can get inflamed, preventing smooth gliding of the tendons as the muscles contract or the wrist bends. However, the cause is the same; repetitive use of the thumb with a sideways movement of the wrist. Overloading these tendons causes them to swell, reducing the space in the sheath, leading to pain and stiffness.
Hip
The gluteus muscles are a group of three muscles that make up your buttocks. Gluteal tendinopathy causes pain in the side of the hip and is common in runners and inactive people. Pain here can be caused and aggravated by sleeping on your side, sitting with legs crossed and running with a gait that crosses the midline on contact. Gluteal tendinopathy pain will increase slowly over time and will be accompanied by stiffness, however, range-of-motion should not be decreased.
Knee
The patellar tendon attaches your quadriceps to your knee cap and down to your shin bone. Patellar tendinopathy usually occurs in younger athletes (15-30yrs) who repetitively load the tendon through jumping, suddenly stopping or changing of direction. Sports such as basketball, tennis and football commonly cause patellar tendinopathy. The pain will be felt in the front of the knee, commonly below the kneecap.
Ankle – Achilles
Achilles tendinopathy can happen in two places, 1) where the tendon joins to the ankle, or 2) where the tendon turns to muscle (called the musculotendinous junction or MTJ). Achilles tendinopathy is hallmarked with morning pain that slowly gets better the more you walk around. This is because the tendon has to perform to full range of motion with basic movements such as standing and walking, stretching and irritating the tissue. Swelling will be minimal – however the affected tendon will be thicker in diameter and may have a painful nodule compared to the unaffected side.
Tendinopathy treatment
While the location of tendon injuries is variable, the approach to treatment is the same:
- Offload: Give the tendon a period of rest. Spend time stretching other muscles around it, but not the affected muscle/tendon. For example; rotator cuff tendinopathy could involve stretching the chest muscles (pec major/minor) and back muscles (latissimus dorsi) to encourage optimum shoulder positioning and movement.
- Gradually load: Eccentric exercises have proven results in helping the tendon to remodel and increase tolerance and strength. Eccentric exercises involve the muscle lengthening while contracting – eg: bicep curl in reverse. Progressing to weight/multidirectional/fast-twitch muscle fibre training. Your practitioner can help guide you with exercises for your specific injury.
- Movement/biomechanics: Changing the way we move works on the root cause of the problem and can help prevent recurrent injuries. For example, a runner's gait can have a big impact on how much the Achilles tendon is loaded.
- Manual therapy: Most importantly, an osteopath/physio can help guide you in the above approach to treatment. They can also provide you with some relief from pain and promote tissue healing through massage techniques and acupuncture – helping you to achieve your goals and get back to doing what you love.
- Other: Shock-wave therapy, laser therapy, platelet-rich plasma or corticosteroid injections – these modalities are all used in the treatment of tendinopathy with varying results. Your practitioner can explain them all and help refer if needed.

Summary
While we don’t know everything about tendinopathy treatments, here are some undeniable truths that every patient needs to keep in mind:
· Rest alone is not the answer. It may settle and reduce the pain in the interim but returning to activity is often painful again. This is because rest does nothing to increase tendon load tolerance.
· Tendinopathy is not considered to have a classic inflammation response. That being said, research has found that ibuprofen is helpful in the early stages to assist in tissue repair.
· Those with a predisposition to tendinopathy may find that even a subtle change will cause a flare-up, which will then take a long time to heal.
· Reducing the load initially to settle the pain is important. A short-term reduction in the aggravating movement/compression is required.
· Research has found that the best treatment for tendinopathy is exercise. Sorry people, but if you want to get better you will need to do the exercises you practitioner gives you. A lot. For longer than a week. Tendons need to be loaded slowly and progressively to increase their tolerance to load. In most cases, a tendon will continue to be painful and repetitively flare up if this crucial stage is missed.
· Similarly, tendinopathies rarely heal with passive treatments alone. By this I mean, just getting osteopathic treatments/injections/shockwave therapy/acupuncture will not fix your issue. In fact, multiple injections have been found to disrupt the healing process!
· Everyone is different. Everyone moves differently, places different strains on their body, has different predispositions, tolerates pain differently. Therefore, exercise needs to be individualised.
· As per our blog post on imaging: the diagnosis on imaging is not equal to the pain you feel. Some people have tears, tendinopathy, calcifications and are asymptomatic. For this reason, treatment focuses on your improving pain levels and function rather than sending you off for repetitive imaging to check on tissue healing.
· Most importantly, remember – Tendons heal slowly. They respond very slowly to exercise and you need to have patience. It may be tempting to resort to the ‘quick fix’ of an injection or surgery, but in reality, there is no easy way out. Put the time and effort in and you will feel better eventually.
References
(J. L. Cook, Rio, Purdam, & Docking, 2016; J. Cook & Purdam, 2012; Coombes, Bisset, & Vicenzino, 2010)
Cook, J. L., Rio, E., Purdam, C. R., & Docking, S. I. (2016). Revisiting the continuum model of tendon pathology: what is its merit in clinical practice and research? British Journal of Sports Medicine, 50(19), 1187–1191. https://doi.org/10.1136/bjsports-2015-095422
Cook, J., & Purdam, C. (2012). Is compressive load a factor in the development of tendinopathy? British Journal of Sports Medicine, 46(3), 163–168. https://doi.org/10.1136/bjsports-2011-090414
Coombes, B. K., Bisset, L., & Vicenzino, B. (2010). Efficacy and safety of corticosteroid injections and other injections for management of tendinopathy : a systematic review of randomised controlled trials. The Lancet, 376(9754), 1751–1767. https://doi.org/10.1016/S0140-6736(10)61160-9
Gattie, E., Cleland, J., & Snodgrass, S. (2017). The Effectiveness of Trigger Point Dry Needling for Musculoskeletal Conditions by Physical Therapists: A Systematic Review and Meta-analysis. Journal Of Orthopaedic & Sports Physical Therapy, 47(3), 133-149. doi: 10.2519/jospt.2017.7096
Liao, C., Xie, G., Tsauo, J., Chen, H., & Liou, T. (2018). Efficacy of extracorporeal shock wave therapy for knee tendinopathies and other soft tissue disorders: a meta-analysis of randomized controlled trials. BMC Musculoskeletal Disorders, 19(1). doi: 10.1186/s12891-018-2204-6
Miller, L., Parrish, W., Roides, B., & Bhattacharyya, S. (2017). Efficacy of platelet-rich plasma injections for symptomatic tendinopathy: Systematic review and meta-analysis of randomised injection-controlled trials. BMJ Open Sport & Exercise Medicine, 3(1), e000237. doi: 10.1136/bmjsem-2017-000237
Tumilty, S., Munn, J., McDonough, S., Hurley, D., Basford, J., & Baxter, G. (2010). Low Level Laser Treatment of Tendinopathy: A Systematic Review with Meta-analysis. Photomedicine And Laser Surgery, 28(1), 3-16. doi: 10.1089/pho.2008.2470
The post Tendinopathy Treatment – Overuse injuries and pain reduction appeared first on MetaMed.
]]>The post Imaging – Help or Hindrance? appeared first on MetaMed.
]]>Modern Day Medical Imaging.
Modern imaging techniques such as X-ray, ultrasound, MRI and CT Scans have the ability to show us anatomical structures in great detail. Since the inception of medical imaging, vast improvements have been made on clarity and availability; providing medical practitioners and patients with a clear diagnosis. A clear diagnosis can help to guide practitioners to give you a clear prognosis and management plan, whether this is a broken bone, internal bleeding, head trauma, or a tumour.
My Experience
After recently breaking my wrist (again) and going in for an x-ray, I realised that many would not be aware of the risk associated with x-ray and CT scans. Had I not known this already, I would be completely unaware that a single x-ray can increase your risk of cancer (1). CT scans are also problematic, with even higher levels of radiation. Areas such as arms and legs require a much lower radiation strength and therefore the risk is less. However, the spine or chest with its many layers of bone, muscle and organ require a higher strength scan, resulting in increased risk (1). Fortunately, ultrasound and MRI scans are safe. However, ultrasound cannot read bones, and MRI is very costly.

Hunting For A Diagnosis
When in pain, the desire to get a diagnosis is strong. For example, those with an old shoulder injury that just won’t heal will often go to their doctors pleading for an x-ray or ultrasound. Similarly, back pain can be debilitating and those suffering become desperate for an answer. However, you have to weigh up the pros and cons. What benefit will come from getting a diagnosis? Once you have a diagnosis – will your management options change?
Does Getting An Image Change Treatment?
Have you been diagnosed with shoulder impingement or tendinopathy? Have you been scanned, given the injection and in 8 weeks’ time the pain has come back? Here, the treatment you would receive from an Osteopath would be the same pre and post-scan/injection – the management doesn't change. Osteopaths use a variety of diagnostic tools including the same active tests a specialist would use, considering the injury cause and looking at your individualised anatomical makeup. In doing so we can diagnose and treat with great results and no unnecessary scans or injections required.

Here's An Example
The Conservative/Treatment Path
Shoulder pain or back pain are great examples of injuries that should be treated conservatively initially. ‘Conservative treatment’ includes seeing your local Osteopath, Acupuncturist or Physiotherapist for treatment, taking recommended supplements, attacking an exercise regime with focus by regularly doing the stretches provided.

The Specialist Path
The non-conservative pathway is seeing a specialist, getting a scan and putting a name to your disorder. The specialist will likely recommend getting a corticosteroid injection, nerve block injection or having surgery. These treatment options are invasive, have varying results and don’t address the reason why the injury happened in the first place (2–4). Not to mention the side-effects of steroid injections; steroid injections have been found to slow healing in the tendon (5).
What The Studies Show
Over imaging is an endemic in healthcare. Studies have shown that unnecessary imaging and diagnosis hunting can lead to poorer health outcomes and higher levels of disability (6). There is growing evidence that pain has a strong association with stress levels, poor sleep, anxiety/depression and negative beliefs around pain. Indicating that all aspects of your life need to be addressed when treating pain – something we strive to do at MetaMed. We help guide you to de-stress, sleep better and become more trusting of your body and its strength, resulting in a more positive future outlook. We actively refer within the community to find you the right trainer/practitioner to support you back to feeling 100%.
To Sum It All Up
Getting a diagnosis from medical imaging is not the be-all and end all to your issue. Studies have shown that people who are pain-free often have ‘abnormal’ findings when given an MRI. In this study 91% had disc degeneration (loss of height in your spinal discs), 56% had disc bulges, 32% had disc protrusions and 38% had annular tears (the ligament around the spinal disc) (6). Yet these people all reported no back pain. Similarly, people with shoulder impingement, bursitis or tendinopathy often have similar if not worse findings on the unaffected side. When scanned, 95% of asymptomatic patients were found to have ‘abnormal’ findings in their shoulders (7). Which leads us to the conclusion that the pain you feel doesn’t necessarily correspond to the ‘abnormal’ findings that imaging may provide. In these cases, one may get little or short-lasting relief from nerve blocks, steroid injections or surgeries.

The main takeaway message here is before you go searching for a diagnosis, as it can have a negative impact on your health. Instead, give the conservative treatment a try. Focus on what combination of treatment/exercise makes you feel better. Radiological imaging should only be used when there are clear indications to do so and once conservative treatment options have been exhausted.
Written by Anna Burgess, Osteopath @ MetaMed · WANAKA
References
1. Harvard Medical School. Radiation risk from medical imaging – Harvard Health [Internet]. 2018 [cited 2019 Jan 30]. Available from: https://www.health.harvard.edu/cancer/radiation-risk-from-medical-imaging
2. Cook T, Minns Lowe C, Maybury M, Lewis JS. Are corticosteroid injections more beneficial than anaesthetic injections alone in the management of rotator cuff-related shoulder pain? A systematic review. Br J Sports Med [Internet]. 2018 Apr 1 [cited 2019 Jan 30];52(8):497–504. Available from: http://www.ncbi.nlm.nih.gov/pubmed/29305377
3. Carofino B, Chowaniec DM, McCarthy MB, Bradley JP, Delaronde S, Beitzel K, et al. Corticosteroids and local anesthetics decrease positive effects of platelet-rich plasma: an in vitro study on human tendon cells. Arthroscopy [Internet]. 2012 May [cited 2019 Jan 30];28(5):711–9. Available from: http://www.ncbi.nlm.nih.gov/pubmed/22264830
4. Jordan JL, Konstantinou K, O’Dowd J. Herniated lumbar disc: injection interventions for sciatica. BMJ Clin Evid [Internet]. 2016 [cited 2019 Jan 30];1118. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4747321/
5. Coombes BK, Bisset L, Vicenzino B. Efficacy and safety of corticosteroid injections and other injections for management of tendinopathy : a systematic review of randomised controlled trials. Lancet [Internet]. 2010;376(9754):1751–67. Available from: http://dx.doi.org/10.1016/S0140-6736(10)61160-9
6. O’Sullivan P, Lin I. Acute low back pain: Beyond drug therapies. Pain Manag Todayanagement Today. 2014;1(1):8–13.
7. Girish G, Lobo LG, Jacobson JA, Morag Y, Miller B, Jamadar DA. Ultrasound of the Shoulder: Asymptomatic Findings in Men. Am J Roentgenol [Internet]. 2011 Oct 20 [cited 2019 Jan 31];197(4):W713–9. Available from: http://www.ajronline.org/doi/10.2214/AJR.11.6971
The post Imaging – Help or Hindrance? appeared first on MetaMed.
]]>The post Why Do I Need Treatment if I’m Not in Pain? appeared first on MetaMed.
]]>People often think to only seek treatment or therapy when they are in pain.
Most of us feel niggles and strains, and we recover. Other times we feel them and we hope they'll get better on their own… but then they keep getting worse, and interfere with your day, work or life in general. That's a real pain!
You might take the odd pain killer, because that's easier…
It works for a while…
But then they stop working!
By the time you are in pain, your body has already reached crisis point. That's why it's screaming out to you to do something.
Our Body Is Capable, Until It's Not
Our body does an amazing job at compensating, meaning it can hold things together and keep working even when things aren't quite right, but if you stress it too much physically, emotionally, mentally it can only handle so much. Everyone has different thresholds, some greater than others.
So often we don't see people until they're in pain, but the issue may have been brewing for many days, weeks or months just waiting to rear it's head.
Our initial focus is to get you out of pain. This is when you can think clearer, move freer and get back to doing the things you love.
The Vicious Cycle
So many people feel great after two or three treatments then decide they don't need anymore. We love that feeling too, but unfortunately, we see the following pattern reoccur.
- You come in for pain…
- You feel better after a couple of treatments…
- You decide you don't need any more treatments…
- Then a few weeks later your pain starts to slowly creep back in…
- It gets intolerable…
- You feel like you're never going to get better…
When you get into the thought that you're never going to get better, that's not a nice place to be.
Your Body Like an Iceberg
In the above video, Dr. Auria Young our holistic chiropractor discusses how your body is like an iceberg. This is how we can best explain why your pain comes back when you stop treatment.
Your pain is everything you see above the water. Over time you have physical therapy and chip away at the painful areas. You feel great once you can no longer see the iceberg.
But look at how much is brewing under the surface, waiting to build up again.
So when you get to the water level, you're not in pain. The reason we recommend maintenance treatment is to keep chipping away at what is below the surface. To get to the root of the issues so that your problems take longer to arise again.
Maintenance Treatment
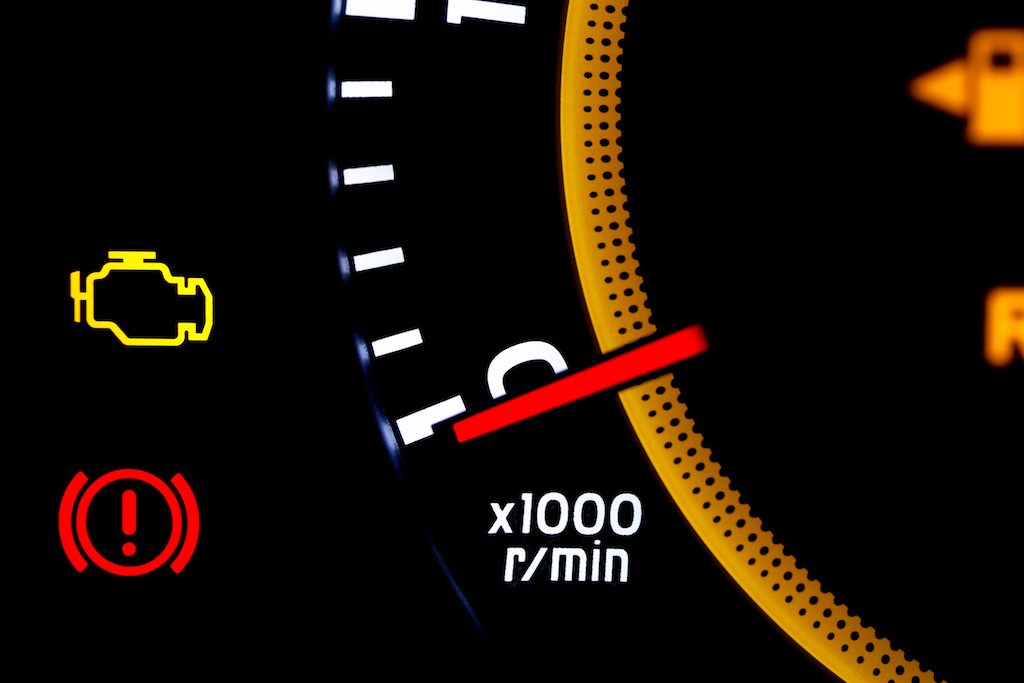
You've probably heard this term over and over again. And the analogy of the car. If not, here it is again.
Think about how you look after your car, taking it for regular WOFs and servicing (hopefully) so it keeps running to get you from A to B. If something doesn't sound right, or a light flickers on your dashboard, you go get it checked out. Because you need your car to keep working for you!
If you ignore the sounds and the lights, it may keep going for a little while. However, one issue may have a knock-on effect to another area of your car. It keeps going… until it can't anymore.
If you look after your car. Look after your body as your vehicle, to run efficiently, get you from A to B and make life easier!
If you don't look after your car, you may have to rethink things a little. Do you not look after your car, just like your body?
Do I Have to Keep Coming in Forever?
People come in depending on how long their body can hold a treatment. Various factors are involved and is entirely different for everyone.
Things that can impact:
- Stress – mental and physical
- Lifestyle
- Diet
- Environment
We aim to have you independent of treatment as much as possible. This may mean you need to make changes in lifestyle and stress situations that you are able to change. It may also mean you need to engage in stretches or rehab exercises, start a new activity to support your body.
People can come in from anywhere between every three weeks to 3-4-6 months!
The best part is they come in feeling great, become more aware of their body holding tension and reduce the rate of injury, or recover much faster from injury.
Self-Care
Allowing yourself to get treated is a great self-care tool. It keeps your mind-body balance, keeps you going and doing what you love.
The post Why Do I Need Treatment if I’m Not in Pain? appeared first on MetaMed.
]]>The post 5 Tips to Prevent Headaches and Migraines appeared first on MetaMed.
]]>Headaches and migraines aren't just a pain in the head. They're a pain in the butt. Suffering from daily, weekly or even random headaches can significantly interfere with your day and ability to do simple tasks.

Headaches and Migraines Can Affect Your:
- Ability to work
- Focus
- Decision making
- Ability to look after your kids
Although headaches and migraines are slightly different (see our post on Migraines) there are some basic tips to help prevent and manage them.

Top 5 Tips to Prevent Headaches and Migraines:
- Keep your hydration up. Drinking at least 2 litres of water per day. If you have difficulty drinking water you can try sparkling water, a squeeze of lemon, or drinking non-caffeinated herbal teas. Herbal teas are a great option during the cooler months. Try peppermint, berry teas or relaxing blends. Avoid sweetened drinks, soft drinks or energy drinks.
- Eat regular and small healthy snacks and meals. This helps to keep your blood sugar levels up and help sustain energy. Keep sugar content down in your snacks and meals to avoid a sugar crash and tiredness later. High-fat snacks such as avocado, salmon, nuts. It is also a good idea to identify if you have any particular foods that trigger headaches or migraines and avoid these.
- Regulate your sleep and wake times (read our blog post on Benefits of Regulating Your Sleep Cycle). Sleep is an important part of winding down from your day and repairing from any stressors you may have encountered. Try and go to bed by 10pm and avoid screen time for 30- 60 minutes before bed.
- Stress relief. Finding ways to let go of daily stress helps relieve muscle tension and wind down for a peaceful nights sleep. Meditation is one way. Going to a yoga or exercise class is another. If you have difficulty meditating there are guided meditation apps with some great sleep stories, such as Calm App.
- Magnesium supplements are great for relaxing muscle tension and calming your nervous system and can aid with reducing frequency and intensity of headaches and migraines. Read more about Magnesium types and doses here.
We are here to help
The post 5 Tips to Prevent Headaches and Migraines appeared first on MetaMed.
]]>The post Arthritic Neck: Chiropractor or Osteopath for neck pain appeared first on MetaMed.
]]>Have You Been Told You Have Arthritis in Your Neck?
Arthritis is another word for:
- degeneration
- wear and tear
We often find that people who have a stiff and sore neck are being told they have arthritis, and there is nothing you can do about it. That it's just part of ageing. True that it's part of ageing, but not true that you can't do anything about the pain! Especially if you haven't tried hands-on treatment.
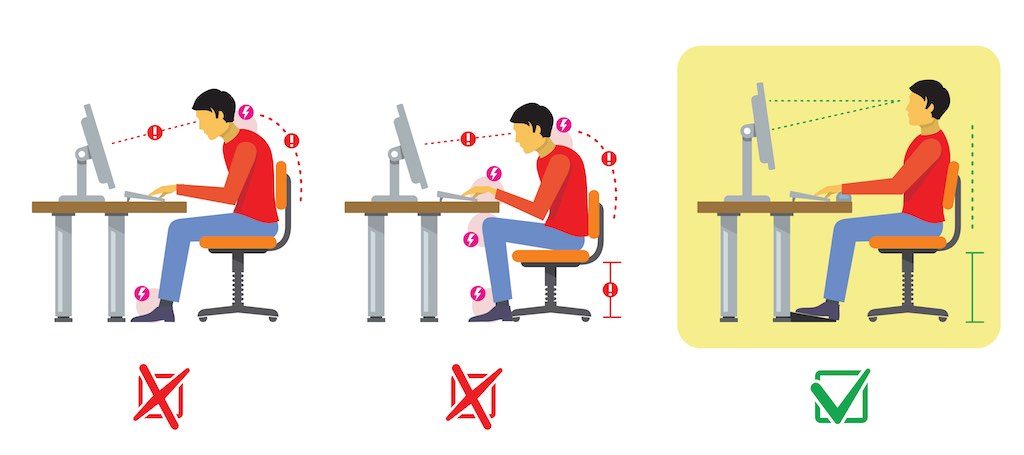
You may have been referred for x-rays which show a little bit of joint space narrowing and words used such as spurs or osteophytes (little bony growths). But the images of your neck don't necessarily correlate with your level of discomfort, AND x-rays only show us the state of your bones. What it doesn't show is the state of your muscles. It doesn't show if they are tight or contracted.
These tight muscles are often the cause of a lot of discomfort in people with ‘arthritic necks'.
So please don't let these words or the images of your neck scare you away from trying to help yourself.

Degeneration is Normal
Some degree of arthritis or degeneration is normal. There are different factors that may contribute to your level of degeneration in your joints.
- previous trauma may predispose to earlier degeneration
- posture affecting how much load certain joints take
- higher levels of physical
labour in your job - sedentary jobs that require long periods of sitting
Different Types of Arthritis
Normally when someone
The signs and symptoms of a wear and tear type arthritis vs. autoimmune tend to be quite different. Something a health care professional is normally able to pick up.
People often remember an older relative who may have had a more aggressive type of arthritis such as rheumatoid or ankylosing spondylitis that has caused a deformity in the joints, and worried they will end up like that when told they have arthritis.
It is important that you clarify which type of arthritis you have.
What You Can do to Help?
- Posture improvements. Download our OFFICE ERGONOMICS sheet.
- Stretch your neck regularly. Download our NECK STRETCHES sheet.
- Strengthen to improve your muscle endurance. You may want to seek professional advice around what strengthening exercises are best suited to your needs.
What Can an Osteopath or Chiropractor do?

Osteopaths look at the whole body and not just your symptoms. We always go through a thorough history with you to determine the history behind your discomfort. Everyone experiences pain differently so we want to get your perspective on what is going on. We also go through past medical history and a general overview of your lifestyle to determine any underlying issues, and to educate you about beneficial changes.
We then examine the area to see how you move and how your muscles feel. At the same time, we can do certain testing to rule out any other issues that may be contributing to your neck pain.
So if you have neck pain, it's important to address the front and back of your neck, as well as all areas related ie:
- Shoulders
- Chest
- Upper back
- Pelvic and hip posture and alignment
- General core activation and endurance
- Overall posture
- Ergonomics
You can see there is more than just focusing on where you have discomfort.
Treatment Often Involves:
hands on soft-tissue massage work- cupping or dry needling
- gentle joint articulation
- joint manipulations if it determined to be safe and beneficial for your condition
- prescriptive stretches and exercises to help maintain you between treatment
How Often Do you Need Treatment?
It varies between individuals but our general aim is to reduce or resolve pain as much as possible. If you have had the discomfort for months or years we can still help reasonably quickly.
As your symptoms improve and pain diminishes we aim to spread your treatments out as much as possible. This may require you to keep up with regular stretches or exercises in between.
Once you feel easier movement and less discomfort you're usually in a better headspace to take on postural advice and start to make necessary lifestyle changes to avoid further stress or load to your joints.
Chiropractor Or Osteopath: Who Should You See?
Either! At Metamed we have both chiropractic and osteopathic practitioners that provide very similar treatments. Both are experienced in anatomy and know the spine well. You’re in safe hands with both chiropractors and osteopaths at Metamed.
Frequently Asked Questions
Differences Between An Osteopath And A Chiropractor?
Every practitioner treats differently. Each and every osteopath will be different, as well as each and every chiropractor. It’s really about trying different people and seeing what approach works best for you. After completing our training at university, every practitioner has to complete Continued Professional Development courses, allowing them to diversify and specialise in different areas. At Metamed, we use functional movement, acupuncture, emotional anatomy and herbalist advice on top of our skills as osteopaths or chiropractors.
Often appointment times differ between clinics, at Metamed our initial appointment is 1 hr and follow up appointments are 30mins, providing us with ample time to get to know you and your issue and treat accordingly. These appointment times are the same for all of our practitioners.
Can neck pain be a sign of something serious?
Generally no. Our team is trained in being able to identify any serious signs and symptoms and can refer on to your GP if need be.
Can osteopathy help trapped nerve?
Yes! Definitely! Trapped nerves are a result of narrowing vertebral disc space or lesions that have built up around where the nerve exits the spine.
References:
- Ministry of Health https://healthcentral.nz/latest-statistics-indicate-more-kiwis-living-with-arthritis/
The post Arthritic Neck: Chiropractor or Osteopath for neck pain appeared first on MetaMed.
]]>