The post Chiropractic Care In Pregnancy appeared first on MetaMed.
]]>Why is Pain Common?
The female body is amazing at adapting to the growing baby. During pregnancy, a hormone called relaxin allows the ligaments in the body and around the pelvis to relax and soften. This allows the pelvis to expand while in labour and accommodate the growing baby. This is a very important process the body goes through and can facilitate more movement through the joints. This increase in movement with the added stress and pressure from a growing baby can lead to inflammation and the sensations of pain.
The most common places pregnant women experience discomfort is at the pubic symphysis (SPD) and the sacroiliac joints in the pelvis. The result spinal, low back pain and pelvic pain.
How to Prevent Pain in Pregnancy
The first trimester is not a common time to experience discomfort but is a great time to get into a good pre-baby care routine. This is the perfect time to prepare by choosing stability and endurance exercises to get the deep core, pelvic floor and pelvic stability muscles working. This helps minimise the stress placed through the spine and pelvis in pregnancy. It will also help make labour easier and help the pregnant mother's body spring back into good shape postpartum.
The recommended exercises will be slightly different to a “normal” routine so it is important to find a professional who can guide you through the different exercises at each stage of your pregnancy. A specialised personal trainer or a pregnancy chiropractor with pre and postnatal management training is essential.
Chiropractic care can start through any trimester and we recommend starting by the end of your first trimester as a preventative approach. It's also a good part of your pre-baby body care routine. It is far better to get into a good routine rather than to wait. But for some, this isn’t an option so chiropractic care can be started as a pain management approach whenever possible.
Benefits of Chiropractic Care During pregnancy
There are many benefits. Chiropractic treatment can make pregnancy more enjoyable, labour easier, and recovery quicker.
Your chiropractor will ensure that your body is well aligned, your muscles are working well, and your posture is balanced. This helps to restore and maintain the proper function of the body.
The added bonus of a well-aligned posture is that the “internal” will also be well aligned. This is not a common topic of discussion but any external misalignment can result in an internal misalignment. Torsion through the pelvis can translate to the womb and cause a torsion through the womb. This can alter the available space and the positions the foetus can adopt. The result can often be a more painful, prolonged labour and uneven pressure distribution through the pelvis, spine and hips.
Treatment is safe and can be done through each trimester of pregnancy. Specialised pregnancy techniques will vary for each stage and can be catered to your needs.
The chiropractic adjustments where you hear the ‘cracking’ are only performed after the first 13 weeks of pregnancy. It is perfectly safe with no known contraindications. We don't recommend doing this on your own. It is a technique that should only be performed by a trained professional.
A good health care and exercise routine will help through labour and will aid postnatal recovery.
What if the Baby is Breech?
If the baby is in a breech position, chiropractic care and other positional techniques have been shown to help the baby turn on its own shortly after treatment. Chiropractors don’t perform external cephalic version (ECV). This is only performed by specialized doctors but there are other techniques that chiropractors can use that have been shown to be safe and effective.
Postnatal Care
Birth is a traumatic process on the body, whether it was a natural birth, c-section or induced labour. The birth process will have major effects on the muscles, skeletal system and the soft tissues in the body. Care after birth can help aid a speedy recovery and get you back to moving well.
Chiropractic care is also safe for the treatment of babies and it is always recommended to get a newborn checked. Ask your paediatric trained pregnancy chiropractor for more details on the benefits.
The post Chiropractic Care In Pregnancy appeared first on MetaMed.
]]>The post Shoulder Injuries appeared first on MetaMed.
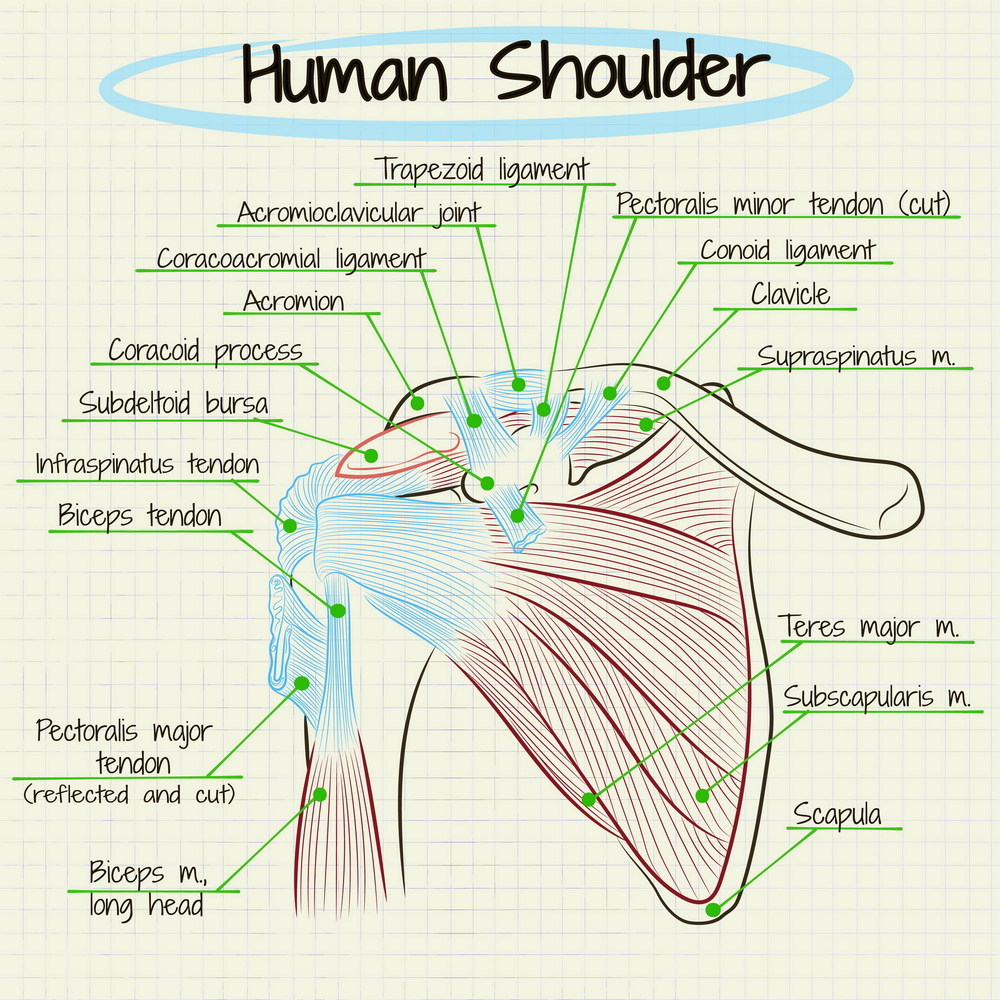
]]>The shoulder is a complex joint, made up of many small muscles (rotator cuff, NOT rotor cuff) that all have a crucial role to play. ‘Crucial’ because the joint is so mobile and has little in the way of supporting ligaments, so the muscles have to be strong to stop your arm flapping about in the wind. If one of these muscles is out of kilter, you are more susceptible to injury and on-going pain. So, a quick anatomy lesson.
Shoulder anatomy 101
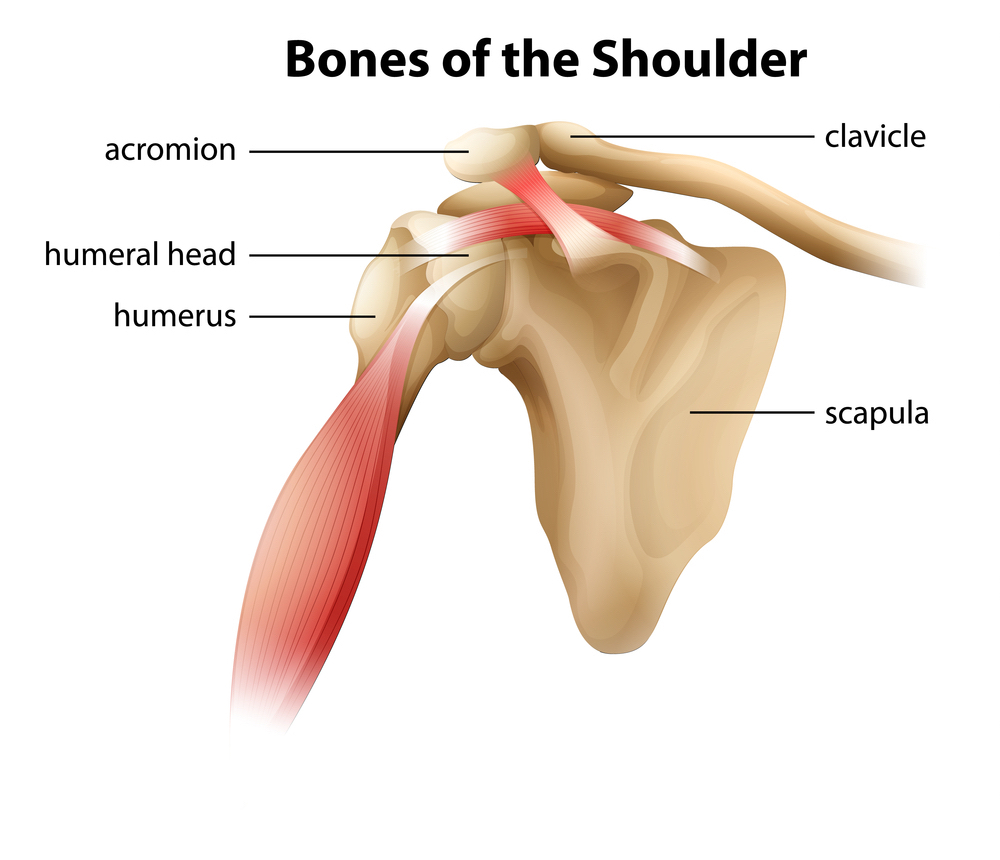
BONES: The shoulder complex is made up of 4 main bones, your humerus, scapula, clavicle and sternum. These combine to make 4 joints that all affect how your arm moves.
LIGAMENTS: The ligaments in the shoulder are small, this allows us increased mobility but sacrifices stability.
MUSCLES: This infamous structure is a collection of 4 muscles: subscapularis, infraspinatus, supraspinatus and teres minor. Good names huh? That’s why we call it the rotator cuff… These muscles are located on the back of your shoulder, with your pectoralis major and deltoid supporting the front.
Rotator cuff tear
What it is – The four muscles that make up the rotator cuff are responsible for keeping the ‘ball in the socket’ and assists in moving your arm. The leading cause of shoulder pain and disability, rotator cuff tears are common in sportspeople and those who do a lot of overhead work. They can be from traumatic injuries or from micro-tears that build up over time and lead to degenerative changes.
What it feels like – pain at night, with overhead activities, weakness and stiffness in the shoulder. Difficulty raising your arm, compensating by hiking through your upper traps in your shoulder. Pain can also radiate down the arm and into the neck.
Treatment
Manual therapy – works on muscle tension that may be affecting the position and mobility of the shoulder blade and humerus causing increased pain at the area. Exercises to strengthen the un-injured muscles and increase stability. Once the injured tendon has healed, focus is put on regaining the ability to activate and strengthen that muscle.
Medical – surgery to reattach the tendon, for complete or large partial tearsonly. This requires a referral to a specialist which your osteopath can organise. Receiving medical treatment before surgery is always a good option to improve your surgery outcomes. Surgery will also depend on how much you use your shoulder in work and sports. Over time your body can compensate even if a muscle or tendon has completely ruptured.
Other – ice/heat, rest, time.
Rotator cuff tendinopathy:
What it is – every muscle is connected to bone via a tendon. Tendinopathy occurs when there is a period of overuse, or increased compression or load. The tendon that is placed under strain fails to fully heal and the result is a swollen and vulnerable structure.
What it feels like – Dull pain that increases over time. Sometimes sharp pain/pinch in the shoulder or lifting your arm overhead. Growing weakness and pain with arm movement/sleeping on it.
Treatment
Manual therapy: Massage to reduce swelling and improve function in the muscle. Injury specific exercises. Advice on asymmetries in training/movement. Strengthening work to ensure other muscles around your shoulder are strong and supportive.
Medical: corticosteroid injections (often doesn’t last for more than a month). If you do opt for this try and get a guided injection to ensure the right spot is targeted.
Other: anti-inflammatories such as ibuprofen. Ice to reduce swelling. Rest from aggravating activities.
Shoulder impingement
What it is – There is a small space (approx. 1cm) underneath your clavicle and scapula called the acromioclavicular joint (see above). In the space runs the tendon to one of the rotator cuff muscles – Supraspinatus. Along with this tendon is a pad called a bursa, which helps the tendon to glide back and forth smoothly. If either of these get irritated (such as tendinopathy or bursitis) and swell up, the tissues get compressed into the small space and cause pain.
What it feels like – pain in the front of side of the shoulder that increases when the arm is lifted. Increased tension in the neck and increased headache frequency.
Treatment
Manual therapy: Conservative treatment of this injury can take up to a year in some cases however a decrease in symptoms is often noticed much sooner. It involves reducing tension in the shoulder/back/neck to encourage optimal function of the muscles and function of the joints. Guided rehabilitation and techniques to increase the space are also provided as well as improving overall strength.
Medical: corticosteroid injection but only once manual therapy options have been exhausted.
Other: rest from overhead activities, shockwave or laser therapy.
Dislocation/instability
What it is – Considering the anatomy explained above, with the lack of ligament and muscle support in the front of the shoulder, it’s no wonder that shoulders frequently dislocated forward (97% of all dislocations). This often occurs when the arm is stretched up in a reaching position. Instability occurs after a dislocation is the surrounding supporting structures have been stretched or torn, allowing the ball joint to ‘pop out’ easily. Nerve and rotator cuff damage can also occur.
What it feels like – If dislocated all movements are painful and the top of the humerus look misplaced. You'll be very limited with your range until the shoulder is relocated. Often people experience dislocations that spontaneously relocate by themselves. This instability can cause the shoulder to ache, feel loose, or vulnerable in positions such as reaching up or reaching up and back.
Treatment
Manual therapy: to help ease any muscular spasms and tension that has developed due to pain in the shoulder. This sets you up well for rehab.
Medical: relocation of joint, surgery to restore stretched/torn structures. Surgery can generally wait until the shoulder has been assessed.
Immobilisation: 3-6 weeks if under the age of 40 and 1-2 weeks if over the age of 40.
Restore motion: Work on slowly restoring full range of motion in the shoulder with specific functional exercises.
Strengthening: exercises introduced to prepare the muscles for a full return to sport/work.
The importance of rehab
As you can see, these injuries often have a long rehab process that requires a combined effort from patient and their manual therapist, with specific exercises and treatments. The amount of effort you put into your rehab, whether it be resting (actually resting) or doing the exercises prescribed, the faster you will be pain free.
If you have a sore shoulder that’s just not going away, book in with one of our practitioners today for an assessment. We are here to help!
The post Shoulder Injuries appeared first on MetaMed.
]]>The post Osteopathic Treatment For The Feet – Does it Work? appeared first on MetaMed.
]]>Your Feet – A Primer
Each foot is made up of 26 bones and 33 individual joints. It’s the foundation of every single movement we do when standing. The dozens of muscles and ligaments in each foot serve to maintain balance and stability through our only contact point to the ground. The feet are not just inert extensions of our lower limbs, they are the vital platform for almost all of our movement, and should be cared for just like any other area when it comes to injury and prevention.
What kind of ankle and foot problems does an Osteopath treat?
The following conditions affecting the foot can be effectively treated by your osteopath
Plantar Fasciitis
A potentially very painful condition that usually begins as a pulling feeling in the heel or the arch of the foot. This quickly turns into a sharp pain which is often worse in the morning or when initially standing up. It’s a complicated and unique condition that is often misunderstood, and therefore often persists for many months. Fortunately, there are many things we can do to help recover faster and even help prevent plantar fasciitis in the first place.
- Avoid standing for prolonged periods, especially on solid floors like concrete. Many workplaces with solid floors now have rubber matting which can help reduce the fatigue of the foot muscles.
- When standing is unavoidable, the right shoes are essential. You should choose a shoe with a softer sole and arch support to suit your foot. If you’ve got particularly high or flattened arches then orthotic inserts may also be useful.
How to treat Plantar Fasciitis
The best way of treating Plantar Fasciitis is to catch it early. 95% of patients will recover well with conservative treatments that include stretching and strengthening. Depending on what biomechanical issues, issues can be limited to the foot. But problems with the knees or hips can have knock-on effects over time and so these areas should be addressed as well.
You’ll likely also need to make some temporary changes to your daily activities to reduce the strain on the foot. At home, icing the sole of the foot can feel great and give some immediate relief. Keep a bottle of water in the freezer and use it to roll the sole of your foot over it for 15-20 minutes.

Achilles Tendonitis
More accurately called Achilles Tendinopathy, this is a type of overuse injury in which inflammation is not a big factor. With Achilles Tendinopathy, the tendon struggles to repair itself fast enough. You feel pain either directly on the heel or just above the heel where the tendon joins the calf muscles. You might feel the tendon is thicker in this area compared to the other side, or you might find a small nodule. Nodules come from poor collagen organisation as the injury struggles to heal. This happens when the tendon is being stressed more than usual. For example, rapidly increasing running distances, increased hill running, overtraining, or poor footwear. Biomechanics can also play a part if you have poor knee, hip or ankle stability, or chronically weak muscles/tendons in the first place.
How to Treat Achilles Tendinopathy
Fortunately, tendinopathies can be treated successfully. Recovery is faster when the injury is managed correctly at an early stage. Initially, there will need to be a period of rest followed by progressive and very specific strengthening exercises. Then the underlying biomechanical issue should be addressed – a vital part of prevention. Continuing to run/jump/overwork your tendon can lead to irreversible changes, degeneration and weakening of the tendon, and is a precursor to a full tendon rupture!
Sprains
Ankle sprains and foot sprains are one of the most common types of injuries. Most active people will have rolled their ankle a few times in their lifetime. It can take quite a while to recover. Each sprain will reduce the amount of stability, making it more and more likely that you’ll sprain it again. And this can lead to chronic ankle instability.
A serious ankle sprain can overstretch the ligaments and can sometimes stretch the tendons around it. The more they stretch, the less stable your ankle will be. Properly diagnosing and treating an ankle sprain in a timely manner is vital to avoid long term complications, re-sprains, and chronic ankle pain. Your rehab will include a lot of strength and balance work to regain proprioception which is absolutely vital for a strong and stable foot.
Heel Pain
Heel pain can have a variety of causes and they all need to be treated specifically. Your pain might have crept up gradually, or might be after an impact or a sprain, but either way, it can be one of the most annoying places to hurt. Possible causes of heel pain include stress fractures, heel spurs, bursitis, or a ruptured fat pad, but by far the 2 most common causes are Achilles Tendinopathy and Plantar Fasciitis.

Trapped Nerve
A trapped nerve can happen in any part of the body. The following are the most common kinds of issues caused by trapped nerves in the foot or ankle.
Tarsal tunnel syndrome
In this painful condition, the Tibial Nerve is compressed and irritated as it goes into the foot. It runs down on the inside ankle, between your ankle bone and another smaller bone, and is held in place by a big ligament – creating a kind of tunnel that it passes through (hence the name). This nerve can get compressed from injuries, such as sprains or fractures, or it can happen over time.
Flat-footed individuals are at risk because the outward tilting of the heel can strain the tarsal tunnel and put pressure on the nerve. Typical symptoms of this nerve entrapment are tingling, burning, pain or pins and needles. Usually, this is felt on the inside of the ankle or the bottom of the foot.
Plantar nerve entrapment
This issue is less common than other trapped nerves and can feel very similar to plantar fasciitis. The main difference is that nerve pain tends not to improve at rest and can increase intensity at night. There is usually chronic burning heel pain which is made worse with stretching and standing.
Morton’s Neuroma
A unique and fairly common condition which is often described as feeling like you have a stone in your shoe. This is caused by a small growth around a nerve between your 3rd and 4th toe, just below the point at which your toes separate from the rest of your foot. Whilst this condition can be quite uncomfortable, it is rarely painful. It’s more likely to affect women as it is often caused by compression of the nerve by tight narrow shoes or high heels.
Gout
Gout is a pain kind of arthritis that can affect any joints (but usually the big toe). It will come on quite quickly and present itself as swelling, redness and extreme tenderness in the affected area. It occurs when the body has excess uric acid in the blood causing tiny sharp crystals to form in and around joints. Usually the body will absorb uric acid naturally, but diets high in red meat, seafood, organ meats, and alcohols such as beer, can increase the uric acid levels.
Other risk factors include obesity, kidney disease, untreated high blood pressure, family history, and being a male age 30-50. Those who are disposed to it can have repeated attacks over the years. Each of which might last anywhere from a few days to a few weeks. Prevention is much easier than treatment for this condition as it usually relies on anti-inflammatories and allowing the uric acid crystals enough time to be re-absorbed by the body.
How do Osteopaths treat foot pain?
It should go without saying that the most important element to treating the foot and ankle is getting the right diagnosis! Most conditions have very specific needs when it comes to recovery, but there are a number of things that an osteopath will usually consider regardless of the type of injury:
- Movement: Does the foot move like it should? Does it move too much? Simple questions give us big clues about how your joints and muscles will are functioning. A hypermobile joint might mean instability or indicate previous sprains. A restricted joint could be a result of a dysfunction in your gait. Knowing how your joints move gives us an idea of which parts have been under increased load. We can then use a range of techniques including gentle manipulation (cracking) to increase mobility, or alternatively help you strengthen weaker areas.
- Muscles: In the ankle, muscles play a vital role in balance and stability; they make the micro-movements to keep us standing upright. But these muscles are prone to injury whenever the foot or ankle is injured too. We use a combination of soft tissue techniques, cupping, dry needling, and stretching, as well as using exercises to build strength and balance.
- Compensation from other areas: Issues further up the leg can cause real issues for the foot. For example, a hip rotated outward makes it nearly impossible to walk naturally. Ultimately, it’s your foot that has to take make the compensation because it’s the only contact point to the ground. With most foot/ankle injuries, osteopaths check the knees, hips, pelvis and lower back as well.
- How you stand: Looking at how you stand or walk is a great way to see how your body functions as a whole. Biomechanical issues can be hard to spot when you remain still so your osteopath will ask you to do a range of movements and see how the leg integrates and works together. The aim is to take any unnecessary pressure from the injured area by ensuring you are moving biomechanically as well as possible.
- Your day-to-day life: The goal is to get you back to doing what you love as quickly as possible. So osteopaths will always try to find a way to keep you active through your recovery. This might be through certain activities, specific rehab exercises, or even modifying existing activities to help you avoid aggravating your injury. Your osteopath will advise on the best way to continue working and how to avoid making your injury worse by doing so.
The post Osteopathic Treatment For The Feet – Does it Work? appeared first on MetaMed.
]]>The post Osteopathic Treatment For Babies – Safe and Effective Treatments For Newborns & Toddlers appeared first on MetaMed.
]]>Many people think that because a newborn is so young, that surely they cannot have any muscle tension or pain! However, the childbirth process is a stressful experience for both mother and child. As the child exits the birth canal, an extreme amount of force is placed upon him/her to fit through a narrow gap. To allow this to happen, the skulls of newborns are flexible, having not yet fused together. Multiple fontanels or soft spots in the skull allows the bones to overlap as baby passes through the birth canal. Additionally, the baby has to twist and turn while it passes through the body pelvis. Every now and then a baby may have lasting strains and joint restrictions from this process, with tension in their head and neck that results in abnormal head shapes, pressure in the skull or head favouring. Likewise, other areas may also be affected, including the shoulders, back, stomach and pelvis as well as their digestive system
Commonly treated issues include
- Deformational plagiocephaly aka abnormally shaped head from head favouring towards one side, leading to the baby laying its head on one side and in the same position or a prolonged labour
- Muscular torticollis – aka twisted or wry neck
- Breastfeeding/feeding/latching difficulties
- Reflux
- Sleep disturbances
- Unsettled, restless, colicky babies
- Nasolacrimal duct obstruction – aka eye discharge
- Constipation and/or diarrhoea
- Checking for age-appropriate reflexes and hip function
Osteopathic treatment – what does it involve?
Newborns and toddlers respond much faster to treatment than adults. Their muscles relax and their nervous systems calm down quickly, with a very light touch. For this reason, treatment is subtle, gentle and definitely doesn’t feel like a massage that an adult might get. On average, a child will only need to see an osteopath for 2-6 treatments and benefit from long-term results, however, this depends on the reason and cause of the issue and the age of the child.
This gentle treatment will involve looking over your baby so we can check for hip and back alignment and assess mobility. It’s best if your baby is fed and somewhat settled before the appointment – keep this in mind when choosing an appointment time.
Treatment aims to reduce any muscular tensions found, whether this is in the hips, back, shoulders, neck or head. To do this, light soft tissue massage and balancing techniques are used, as well as rhythmic movements to free up joints. No joint clicking/cracking is done to newborns or toddlers in osteopathic treatment.
Babies cannot directly tell us about their discomfort, instead, they may cry, not sleep and be generally unsettled. Osteopathy can help babies with any physical discomfort, allowing them to really settle into their surroundings. Osteopaths can also help to screen for tongue tie and hip issues, teach you some handy settling techniques and advise mum and dad on best ways to hold/breastfeed for her own comfort.
We can also help with training you how to massage and treat your child, what pressure to use and massage techniques to help with self-care at home.

Cranial Osteopathy
Cranial osteopathic treatment is a gentle yet effective treatment approach that provides long-term results. Cranial techniques usually involves gentle touch to feel the body’s natural involuntary rhythm created by the flow of cerebrospinal fluid through the body’s tissues. There can be areas in the body where the tissues do not move as freely and the movement is “stuck”. With a very light touch, the circulation of the cerebrospinal fluid can be affected and improved, restoring healthy fluid movement to the tissues and bringing balance and ease, which promotes the body’s own self-healing mechanisms to restore health and wellbeing.
Although cranial treatment can be useful for people of all ages and builds, babies benefit greatly from early osteopathic treatment. It is a common belief that babies and children should have no structural strains in their bodies as they are too young to have experienced these, however this is not always the case. Babies are often much more settled following treatment as they are grateful to have the stresses of birth and the position that they were in during in-utero released and removed.
An osteopath who is credited with being one the founders of cranial osteopathy said “as the twig is bent so the tree will incline” (WG Sutherland). What this mean is that if there is a strain that occurs during the early stages of one's life, the body will adapt around this and will grow in
Cranial treatment is suitable for all babies and children and can address a variety of conditions and symptoms.
Before and after treatment
Ideally, your child will be fed and settled prior to treatment. After treatment, you may not notice changes immediately, as the body takes time to adjust to treatment. Much like when adults get osteopathic treatment or a massage, babies may also feel more sleepy or irritable for a few hours afterwards.
Reactions to osteopathic treatment are variable. Often the baby or child is very relaxed afterwards and sleeps well. Other children have a burst of energy following treatment, and then usually sleep well after this. Occasionally, babies are unsettled after treatment. This is temporary and can be due to restrictions not having been able to be fully released if they are severe. Additionally, some babies are just unsettled following treatment as Cranial Osteopathy can feel different from anything they’ve ever felt before.
How many treatments will be needed?
On average two to six treatments are usually enough. This does vary according to the severity of the problem and the age of the baby/child. The younger they are, the less treatment it usually takes. We will be able to give you a better idea of the number of treatments that will be required after talking to you and following the initial treatment.
Mums and Bubs duo appointments
At Metamed we offer Mums and Bubs 60min duo appointments which are ideal during the first 3 months postpartum. This provides ample time to give both baby and mum a treatment after the marathon of birth.
These appointments are excellent for addressing any strains or structural restrictions that a baby might be carrying post-birth, whether it was a difficult birth or not. Helping to ease common complaints such as sleep disturbances, reflux and an unsettled baby.
Meanwhile, mum can also get some much needed TLC. Your body has gone through so many changes in a short period of time, from being a pregnant woman to a new mother in 9 months! We adopt so many new positions as a new mum; breastfeeding, rocking baby to sleep, carrying the carseat – all of these can cause pain and discomfort that’s unnecessary.
Our duo appointments are available exclusively with our Osteopath Franca Bauer. Franca combines both structural and cranial techniques, as well as offering support on feeding and latching issues and providing straightforward tips and tricks that you can use at home.
You can book in with Franca at our Wanaka clinic, located at 25a Russell Street, Wanaka 9305. Book online here, or call 03 443 2628.
Appointments available: Monday – Friday 8.00 am – 8.00 pm
How to choose a good osteopath for your baby
Things To Consider When Choosing An Osteopath For Children.
As of 2021, all Osteopaths are required to have undertaken extra paediatrics training at the Ara Institute of Canterbury – if not, they are not allowed to treat anyone under the age of 16.
Other than the required qualifications, a good Osteopath will be fluid with treatment, working with the movements and needs of your baby. Osteopaths that treat babies generally have a soft touch, need to be calm during treatment and confident handling and interacting with babies and toddlers.
The post Osteopathic Treatment For Babies – Safe and Effective Treatments For Newborns & Toddlers appeared first on MetaMed.
]]>The post Osteopathy vs. Physiotherapy – What’s the difference? appeared first on MetaMed.
]]>The Truth About Osteopaths and Physiotherapists
The best practitioner is the one that suits your needs
No two practitioners, whether an osteopath or a physio will approach a problem the same way. There are often many routes to the desired destination. Sometimes the practitioner’s route will resonate with you and sometimes it won’t. So it’s important to find a physio/osteopath that fits well with you, your beliefs and your goals.
There are good and bad practitioners
Just like in any profession, there are good and there are bad practitioners. The key is to find a practitioner that is passionate, is continually learning, uses their time well and supports you to achieve your goal/s.
Know your strengths and your limitations.
Here at Metamed, we work closely with local physios and often refer to each other when we feel another profession will benefit you more. We work hard to nurture this relationship and remove the competition. In Queenstown and Wanaka, we are lucky to have physios that specialise in areas such as concussion, hand therapy, cancer rehab, vocal physio and the pelvic floor (to name a few) that we often refer our patients to.
What are the key differences?
Osteopathy and Physiotherapy are very similar concepts. Both are manual therapies that treat musculoskeletal problems. ‘Musculoskeletal’ refers to muscles, tendons, ligaments, bones, and fascia. Both undertake years of training in anatomy, physiology and pathology.
The level of “Continued Professional Development” required to maintain registration means the skills learned after university continue to blur the lines between Osteo and Physio. Osteopaths will become personal trainers, exercise and movement coaches or specialise in functional movement. Physiotherapists will train in specialised joint manipulations (‘clicks’) and holistic, body-wide approaches.
The biggest difference is the philosophy behind the treatment and why we choose the treatment approach we provide.
Osteopathy
Views the whole body as a unit, which is why when you come in for elbow pain, we might end up treating your shoulder and pelvis. To do this, osteopaths study biomechanics, have a deep understanding of anatomy and consider lifestyle factors that may be contributing. There are four osteopathic principles:
- The body works as a single unit of mind, body and spirit. Which means everything is connected and needs to be considered.
- The body has an innate self-healing capacity – the immune system is pretty incredible we think! Given the chance, with the right encouragement, most injuries will heal. This is what Osteopaths specialise in.
- Structure and function are inter-related and require balance. For instance, if you’re all strength and no mobility/flexibility, movement patterns will change, load will be placed on structures it shouldn’t and injury will occur.
- Prescribed treatment should consider all of these things, and be based on the body’s self-healing mechanism, structure and function.
Physiotherapy
Closely aligned with the medical model of health. The focus is more on the problem area presented and treatment of that area. The Physiotherapy profession prides itself on remaining current with scientific research and works closely with hospitals and medical centres.
Physiotherapists are taught to follow treatment protocols and provide rehabilitative exercise-based treatment. A physiotherapy session may be a lot less ‘hands-on’ than an Osteopathy treatment; instead, the focus is a rehabilitative exercise-based treatment that aims to build you back up to your best after injury.
Frequently Asked Questions
What techniques or approaches do Osteopaths use but Physiotherapist do not?
There are a lot of techniques that cross over between Osteopaths and Physiotherapists. However, Osteopaths and Chiropractors are the only practitioners allowed to manipulate (click) the top joint in the spine. Unless they have done specific training, a lot of Physios won’t manipulate joints at all.
Is Osteopathy better than Physiotherapy?
Despite the differences in philosophy, the aim of both treatments is to help relieve your pain. Both are manual therapies that offer a lot of the same techniques. It all comes down to how they are applied and what works best with your body. For example; some people hate being massaged or having their joints clicked, others never do their exercises or rehab. It all depends on you and your relationship with the practitioner.
Do Osteopaths do massage?
Yes, osteopaths offer massage treatments. There are many different approaches to massage, Osteopaths are taught inhibition, cross-fibre, longitudinal and balanced ligamentous tension release, to name a few. Osteopaths have ‘borrowed’ many techniques from other professions, at times modifying them or their application to work within our philosophy. However, a good osteopath clinic will have developed a close working relationship with a massage therapist and refer to them as required.
Is osteopathy good for back pain?
Osteopathy is great for back pain However, osteopaths treat more than just back pain. Any injury, ache or pain – try an Osteopath and see if they can help.
Can an osteopath help with nerve pain?
Yes, but this depends on the cause. Nerve pain from compressions – such as a herniated disc, carpal tunnel or thoracic outlet syndrome can be helped greatly from osteopathy treatment.
Are both treatments good for pain?
Both Osteopathy and Physiotherapy aim to help relieve your pain.
What conditions does an osteopath work on?
Osteopaths can help with any/all musculoskeletal issues. Any injuries (shoulder, knee, hip, back etc), muscle pain, swelling, headaches, digestive issues, jaw clicking/pain, osteoarthritis, rehab post-injury, tendon issues such as tennis elbow or patellofemoral pain, breathing mechanics, pregnancy-related pain.
Can Osteopaths process ACC like Physios?
Yes! Ther's no need to visit your GP or Physio as osteopaths can process ACC. If you have hurt yourself, osteopaths can lodge an ACC claim. Osteopaths have the same access to specialist appointments and x-ray/ultrasound referrals as physiotherapists.
The only difference is that Osteopaths get 16 treatments subsidised under ACC, while Physiotherapists get unlimited treatments.
Most people don’t realise that one ACC claim can be used with different practitioners, including Acupuncturists, Chiropractors, Osteopaths and Physiotherapists.
The post Osteopathy vs. Physiotherapy – What’s the difference? appeared first on MetaMed.
]]>The post Osteopathic Treatment for Sciatica and Disc Injuries appeared first on MetaMed.
]]>Sciatica is a word to describe the pain felt when the sciatic nerve is compressed, inflamed or irritated. The sciatic nerve is the biggest and longest nerve in the body, running from your sacrum (lower back) down the back of your thigh then branching off into your lower leg and foot.
Sciatica is a symptom often caused by disc injuries or from during pregnancy. Disc injuries = disc sprain, bulge, herniation, rupture, prolapse or a slipped disc. If this occurs the disc may cause increased pressure on the root of the sciatic nerve where it attaches to the spinal cord.
During pregnancy, sciatica is caused by the growing baby taking up space and putting pressure on the sciatic nerve. However, referral pain in pregnancy can also be from pelvis instability – which has nothing to do with the sciatic nerve.
Home remedies that help
We often get asked if there’s any quick fixes or home remedies that help with sciatica. I’ve heard of all sorts of weird and wonderful theories such as putting your feet in boiling hot water… Unfortunately, there’s no quick fix!
Alternating a hot/ice pack, using each one for no more than 10mins, switching out 4 times (hot for 10mins, cold for 10mins, hot for 10mins, cold for 10mins) can help with pain relief and promote healing in the area – this can be done 2-3 times a day.
What do disc injuries feel like?
Pain = sometimes people feel pain in their lower back, sometimes not. Sometimes people have neuropathic pain down their thigh, into the calf muscle, ankle and foot, and sometimes they don’t. Neuropathic pain is often referred to as ‘sciatica’, which is actually a symptom/result of nerve irritation and feels like tingling, numbness or diffuse/hard to place pain.
Onset = most of the time a disc will become painful with a minor, seemingly insignificant movement such as bending down to tie your shoe. However, this isn’t something that has happened ‘suddenly’ but is rather a result of long-term movement dysfunction. Often people are dehydrated or fatigued when they hurt themselves, changing the functionality of your muscles and discs. Disc injuries can also happen after a traumatic injury like a car/bike/ski accident.
Can Discs heal by themselves?
Yes. In the UK, studies have found up to 82.94% of disc herniations spontaneously reabsorb, prompting the recommendation of conservative treatment over surgery (1). “Conservative treatment” involves a combination of things that are specific to the patient:
1. Modified everyday movement – this means taking some time off work – and gradually returning. No lifting, twisting, bending for a while to help settle things down. Follow our active rest regime to reduce inflammation and pain. The timeframe around this stage varies greatly from person to person depending on adherence and injury.
2. Physical therapy – can help reduce nerve irritation, increase local blood flow which encourages healing, get your pelvis and mid-back moving efficiently to offload your lower back and provide pain relief to help you carry out your exercises effectively. And definitely no lower back clicks!
3. Specific exercises – there’s no ‘quick fix’ or ‘magical back healing exercise’ that works for everyone. This is body/pain/lifestyle specific and needs to be guided by your practitioner as you heal.
Can I have a disc removed?
Discectomy and spinal fusions have varied results, which depend on the different surgical approaches, patient rehab adherence and individual spinal health. One review of the available research that included 90 studies found that 22% of patients had worsening back pain at their one-year review and up to 23% had a reoccurring disc herniation (2).
In our clinic, we see spinal fusions place more load on the joints above, over time leading to more disc injuries, this is called adjacent segment disease and provides even more reason to make changes to your movement habits.
The osteopathic approach looks at addressing why your disc injury occurred. We encourage specific exercises to help increase mobility in hips, mid-back and shoulders to reduce the strain placed on the lumbar spine. We also teach individual muscle activation and hip hinging to techniques to improve the efficacy of movement. At appropriate times in the rehab process exercises such as Pilates, yoga, swimming and weight lifting.
Physical inactivity is linked to poor spinal health and low back pain
There are so many great gyms and fitness clubs in Queenstown and Wanaka – find one that suits you and get moving! Boxing, weight-lifting, Pilates, yoga, swimming, whatever you enjoy and makes you feel good! This will help to prevent disc narrowing, high-fat content of back muscles making them weak and reduce the recovery time if you do hurt yourself.
NB: if you are lifting weights and performing squats/deadlifts etc, remember to take your time, get your form and breathing sorted and gradually increase the weight.
Disc injuries can cause debilitating pain and have a costly, drawn-out healing time.
But disc injuries can also be totally painless.
Scans on people with and without back pain have found spinal degeneration and disc damage present in both groups (4). Similarly, those in pain can have a disc injury at a different spinal level to what their symptoms would indicate. Confusing indeed.
After a scan, conservative management is usually recommended initially, with surgery being a last resort.
What’s the benefit of a scan?
Scans should be reserved for the obscure pain presentations that your health practitioner is struggling to identify, or for serious presentations/injuries. Most disc injuries present clearly and are easily diagnosed by your osteopath/physio without needing a scan. However, we find that patients don’t take their rehab seriously until their pain is confirmed by a scan. Resulting in unnecessary scans, clogging up the system and increasing wait times.
Where do I start?
Initially, you’ll likely be too sore to do much. Follow our active rest regime to help reduce pain and inflammation.
Then work on increasing your flexibility in your hips and mid-back and strengthening your core and glutes. If you feel any increased pain in certain movements, stop the exercise and consult your practitioner. The sheets supplied are best guided by a practitioner or trainer.
Be patient! Disc injuries can take up to 18months to heal depending on the extent of the injury.
1. Zhong M, Liu JT, Jiang H, Mo W, Yu PF, Li XC, et al. Incidence of spontaneous resorption of lumbar disc herniation: A meta-analysis. Pain Physician. 2017;20(1):E45–52.
2. Parker SL, Mendenhall SK, Godil SS, Bs S, Cahill K, Ziewacz J, et al. Incidence of Low Back Pain After Lumbar Discectomy for Herniated Disc and Its Effect on Patient-reported Outcomes. Clin Orthop Relat Res. 2015;473:1988–99.
3. Teichtahl AJ, Urquhart DM, Wang Y, Wluka AE, O’Sullivan R, Jones G, et al. Physical inactivity is associated with narrower lumbar intervertebral discs, high-fat content of paraspinal muscles and low back pain and disability. Arthritis Res Ther [Internet]. 2015 Dec 7 [cited 2019 Dec 31];17(1):114. Available from: http://arthritis-research.com/content/17/1/114
4. Brinjikji W, Luetmer PH, Comstock B, Bresnahan BW, Chen LE, Deyo RA, et al. Systematic Literature Review of Imaging Features of Spinal Degeneration in Asymptomatic Populations. Am J Neuroradiol [Internet]. 2015 Apr 1;36(4):811 LP – 816. Available from: http://www.ajnr.org/content/36/4/811.abstract
The post Osteopathic Treatment for Sciatica and Disc Injuries appeared first on MetaMed.
]]>The post Breathing Well appeared first on MetaMed.
]]>Why Learning to do it Properly is so Important
It is something we all do thousands of times every day. Whether we are awake or asleep, resting or active; to breathe is to be alive. Whilst most of us don’t take much notice of our breathing, there are a few very important reasons why we should.
- Improves blood flow
- Improves energy
- Supports a strong immune system
- Alleviates stress
Let's just touch on one of the issues most people have in life and how improving your breathing can help.
Stress response
We’ve all been told at one time or another to “take a deep breath” when we have been feeling stressed. As unhelpful and annoying as this can be at the time, there is some sense behind this.
Our “fight or flight” instinct, also known as our body’s stress response, is how we decide to confront or avoid danger. When we breathe in deeply our lungs expand and compress the walls of the heart, restricting blood flow. To compensate, our heart rate increases stimulating this fight or flight stress response.
When we breathe out, the pressure in the thoracic cavity drops and the body relaxes! So, in short, it is the exhale that truly helps us relax, not taking a deep breath in!
This brings us to an issue we see regularly in clinic – people holding their breath in, or not breathing out fully. It's usually the first change when stress is encountered – holding your breath. Over time if we continue this pattern we can keep our body in the ‘fight or flight' response. Stress and anxiety anyone? No thanks.

One Simple Trick to Alleviate Stress
Next time you feel stressed or anxious make a mental note of your breathing. Are you holding your breath? Are your lungs full and chest tight? Taking a moment to forcefully exhale several times can make a big difference and quickly reduce the fight or flight response.
Try This Breathing Technique
Inna Kahzan of Harvard medical school recommends that 40% of the breath cycle is for inhaling, and 60% is for exhaling – so for a 4 second breath in, take 6 to exhale. This ensures not only a full exhale, but also slows the breathing, avoiding risks of hyperventilation which can make that stress response much worse.

Two Ways to Breathe
- Belly breathing
- Upper chest breathing
While breathing is mostly automatic, every breath is not identical. Diaphragmatic (AKA belly breathing) is best for keeping that stress response to a minimum, but unfortunately the stresses of day to day life can lead us to quickly fall into a habit of breathing into the upper chest. This is not ideal, and aside from typically shallower breathing, it can also cause tightening of muscles in the front of the neck and chest over time. If you catch yourself doing this remember the 40/60 rule and EXHALE for longer!
The stress response/breathing relationship is cyclical, so busy lifestyles often feed into poor breathing patterns. However habits form young, and breathing is no exception either. Some of our cultural expectations, such as the wish to have a flat tummy, means we learn from an early age to hold our stomach muscles in tight.
As I’m writing this, I’m trying to breathe deeply into my belly whilst hunched over my desk (like many who work in an office) – try it, it’s practically impossible. This is another great example of the importance of breathing and taking time away from the desk every so often.

If you know poor breathing habits may be contributing to your pain or symptoms come and visit one of our practitioners. If you're unsure we're more than happy to book in a 15 minute complimentary chat to see if we can help you.
Alternatively, if you're not anywhere near Wanaka or Queenstown we also love Emma Ferris the breathing physio from The Breath Effect. She has a great online course and more information on how to retrain your breathing. Click here to find out more information.
The post Breathing Well appeared first on MetaMed.
]]>The post New Year Intentions – Health Resolutions 2020 appeared first on MetaMed.
]]>I'm not one for new year resolutions but I love to reflect and get clear on my intentions. But what do both of these mean? Reflecting and reviewing your year can be a powerful catalyst for change, an opportunity to review what, how and why things have happened. Intentions come from your soul, deep-rooted in your values and what is important to you.
We have a handy workbook to help you work through this. See below to download.
Reviewing your year
Reflecting on the year that was can be hard for some, especially if it was full of things you didn't want to happen in your life. If you're thinking ‘I can't wait until 2019 is over' and you never want to think about it again, you could be missing out on some of the valuable learnings that come from the not so pleasant things you had to face. Learnings and experiences that help shape your decisions in the future to create more of what you do want. Or you may have had a great 2019 and want more of that! So how do you keep creating more of what we want?
Setting intentions
Setting intentions reminds you what is important to you and can help create a foundation of what you say ‘yes' to in your day, week… year. Nurturing and living out your intentions helps you feel more fulfilled in your life because you're usually doing what you enjoy and makes your heart sing. At the same time when you're in the space of living according to your intentions you can positively influence others around you.
A gift for you…
As a gift to you transitioning into 2020, we've created a Create a New Year workbook to help you review the year that was and start or continue to live intentionally and create a path for change in 2020. It's designed to help you look within and…
- REFLECT on the year that was
- ACKNOWLEDGE what did and didn't work for you
- RELEASE any limiting beliefs
- NURTURE yourself
- CHALLENGE yourself to create a great year ahead
- ASPIRE to create change and live the life you want
- ACTION that will move you in the direction you want to go

This isn't goal setting
Don't worry this isn't goal setting (although I am a big fan of goal setting and they can help give you actionable steps to fulfilling your intentions… more to come on that one) this is about coming back to your own truth, acknowledging the blocks (so you can work around them or not encounter them again) and getting clearer on what it is you want to create.
Most of you will be having time off over the Christmas and New Year period, it's a perfect time to reflect. If you thought you had no time during the year and find that thought creep in now (when you've got time off!) stop procrastinating! This exercise doesn't have to take you long. Grab a pen and just write the first things that come into your head. There's no need to overthink these as you already know all the answers.
If you're stuck and need any help filling any section out make a comment below.
May your 2020 be filled with more of what you want and truly desire.
BOOK ONLINE to see one of our practitioners today.
The post New Year Intentions – Health Resolutions 2020 appeared first on MetaMed.
]]>The post Soft Tissue Injury Treatments: Your Options appeared first on MetaMed.
]]>Chronic soft tissue injuries
These types of injury are the result of repetitive stress on a tissue. Commonly known as overuse injuries. See our Tendinopathy post for more details.
Signs and symptoms
Different soft tissue injuries have different signs and symptoms but there is usually some level of redness and swelling, as well as pain and reduced range of motion. There may be some bruising.
Joint-stabilising ligament injuries
Ligament injuries range from mild tearing of a few fibres to complete tears, which can lead to joint instability. The common areas affected are the knee and ankle, but it can also happen around the shoulder, elbow and wrist.
Ligament injuries are graded from 1-3:
- Minor injury with little swelling and tenderness: minor impact on function due to intermittent pain on movement. Grade 1 usually heals in a few weeks, with max strength returning after 6 weeks.
- Ligaments are stretched but intact: some joint laxity (giving way) may be experienced as well as moderate swelling pain and negative impact on function. Grade 2 requires some reduction in use to offload the tissue during the initial phase. Healing may take anywhere from 6 to 12 weeks depending on the injury.
- Complete ligament rupture with excessive joint laxity: Often painful but can also be pain-free due to the destruction of sensory fibers in the injury. Marked swelling and bruising. Painful or inability to weight-bear. Grade 3 requires the opinion of an orthopedic specialist to determine if it requires surgery. A return to normal activity can take anywhere from 4 to 12 months
Muscle Strains
Muscle strains are the same as ligament sprains but in a different type of tissue in the body. Strains happen when a muscle is overloaded and fails, causing tearing of the fibres. We grade muscle strains in the same way as ligaments, from one (mild) to three (severe). Symptoms include swelling, bruising, redness, pain at rest and with movement, inability to use the muscle (moderate to severe only), and muscle weakness.
Treatments for muscle strains depend on the severity of the injury. Initially, POLICE protocol (see below) should be followed. An assessment and accurate diagnosis by an osteopath or physiotherapist will help to determine when and how the muscle can safely be loaded again. The initial rehab starts with low impact movements, followed by a gradual increase in tension. Proprioception and endurance training is recommended only in the advanced rehab stages.
Tendon Injury
Tendons connect muscles to bones and work to transmit forces between the two. The most common tendon pain is from overuse – called tendinopathy. However, acute tendon ruptures also occur.
Tendon ruptures often happen without warning or apparently for no particular reason. The most frequently injured tendons are covered below. A ‘pop’ or a ‘bang’ followed by weakness and pain, is a common sign that a complete rupture has happened. These commonly happen in the achilles in the ankle and the bicep tendon in the upper arm.
Rotator cuff tendon injuries are categorised based on which of the four rotator cuff tendons is affected and the extent of the injury – small/medium/large/complete tear. Symptoms include severe pain at the time of injury, night pain, pain with overhead movements, pain radiating down the arm, and shoulder muscle weakness.
Full-thickness tears require surgical intervention, however, in most other cases conservative rehab is recommended – such as osteopathy, physiotherapy, or acupuncture and specific exercises and stretches.
Bicep tendon injuries often occur after a strong, sudden contraction of the bicep muscle. Similar to the rotator cuff, symptoms include pain in the front of the shoulder, pain with overhead movements, night pain and ‘pop-eye deformity’ – when the bicep muscle, under contraction, appears to rise lower down the arm.
Surgery is generally offered to younger patients that are athletic or require maximal arm strength – Tradesmen, for example. Conservative management is recommended.
A Quadriceps tendon rupture means you will be unable to straighten the knee without help. Some people can walk after injury, some cannot. Graded as either partial or complete.
Partial ruptures require a short period of immobilisation (possibly in a moon-boot) followed by a gradual return to normal activities with specific strengthening exercises. 3-6 week heal time.
A complete rupture calls for surgery, usually in the 72hrs following injury, to reattach the tendon. Following surgery is a period of immobilisation. Depending on the patient and surgeon, rehab will either be conservative (around 4-6 weeks immobilisation) or aggressive (around 10 days immobilisation with exercises included early on). The aggressive approach has produced better results more quickly but it is not for everyone.
People with Achilles injuries often report that the injury felt like someone kicked/stabbed them in the leg, accompanied by a ‘bang’. Other symptoms include swelling in the back of the heel, decreased ability to heel raise or point toes and a palpable gap in the tendon. Achilles injuries are graded 1-4:
- Grade 1: partial ruptures, less than 50% – typically treated with exercises and manual therapy.
- Grade 2: complete rupture with tendinous gap ≤ 3 cm – typically treated with surgery
- Grade 3: complete rupture with tendinous gap 3 to 6 cm – surgery required
- Grade 4: complete rupture with a defect of > 6 cm (neglected ruptures) – surgery required
Rehabilitation
Like the different signs and symptoms, there are also different rehab stages depending on the severity of your injury. Seeking professional guidance after a soft tissue injury will help you to reach your recovery goals faster. Injury specific exercises, massage, joint mobilisation and natural pain relief will speed up recovery and help prevent re-injury.

At-home care
Everyone has heard of RICE: Rest, Ice, Compress, Elevate.
However, I’d like to introduce a new mnemonic, POLICE: Protect, Optimum Loading, Ice, Compression, Elevate.
- P: Protect yourself from further damage by taking an appropriate amount of time off. Have the injury assessed by a professional to find out how long you should rest and when you can return to daily activities.
- O + L: “Optimal Loading” helps to encourage tissue healing, stimulating repair and building strength in the damaged tissue so it can cope with the strains placed on it when you return to your sport/work. Graded loading helps to prevent stiffness, reduce swelling, and reduce pain. Loading an injury is a key element in producing strong tissue that can handle the forces you place on it. This helps prevent future injury.
- I: Ice. Cryotherapy causes the blood vessels in the area to tighten and in doing so reduces swelling, while also reducing inflammation. However, inflammation is part of the natural healing process after a traumatic injury. Icing an injury for long periods of time can cause further tissue damage and prevent optimum healing. We recommend using an ice pack for 10mins at a time, then having a break and coming back to it again in an hour. Remember to wrap your ice pack in a damp towel or cloth to minimise skin irritation.
- C: Compression also helps to reduce swelling and any bleeding at the injury site. A compression bandage (tubigrip) can provide comfort and support to an injury. It should not increase pain or be so tight that the area beneath it turns red/purple.
- E: Elevation increases the return of blood toward your heart, reducing swelling and easing pain by facilitating the removal of inflammation by-products that cause extra nerve sensitivity.
Frequently Asked Questions
What is the best treatment for a soft tissue injury?
This is highly variable and depends on the extent of the injury. What’s important is following the P.O.L.I.C.E protocol directly after the injury, seeking professional advice, and getting an accurate diagnosis.
How long does it take for a soft tissue injury to heal?
Factors that influence the recovery time include the age of the patient, the patient habits such as smoking, and adherence to the rehab protocol.
| Healing Times | |
| Delayed Onset Muscle Soreness (DOMS) | 0-3 days |
| Muscle strain | Grade 1: 0-2wks Grade 2: 4d-3mo Grade 3: 3wk-6mo |
| Ligament sprain | Grade 1: 0-3d Grade 2: 3wk-6mo Grade 3: 5wk-1yr |
| Tendon | Rupture: 5wk – 6mo Tendinopathy: 3wk-12mo |
| Bone | 5wk-3mo |
| Cartilage | 2mo-2yrs |
| Ligament graft | 2mo-2yrs |
Can soft tissue damage be permanent?
Yes. Some ruptures do not qualify for surgical repair and are therefore permanent. However, this is generally only the case when the patient is not in pain or surgeons determine that surgery would non-beneficial or non-successful. Most other soft tissue injuries will heal given the right time and rehab.
Is soft tissue damage painful?
Yes. However, patients often report feeling pain at first followed by a period of no pain when the tissue has fully ruptured.
Is heat good for soft tissue injury?
No. Heat is great for tired or spasmed muscles. Applying heat can also be used as an ice/heat flush if recommended by your health professional. However, acute/new soft tissue injuries should always have ice applied to help reduce inflammation and swelling.
Does massage help soft tissue damage?
Yes. But only after the initial acute phase has passed. Osteopathic treatment can help with repair and healing, reducing swelling, inflammation, pain from compensatory movements and addressing why the injury happened. Your Osteopath will also help to diagnose the injury and guide your rehabilitation. You will get back to your best, pain-free-self faster than if left alone.

The post Soft Tissue Injury Treatments: Your Options appeared first on MetaMed.
]]>The post Are Foam Rollers Worth it? Why & How to use a Massage Roller appeared first on MetaMed.
]]>Is foam rolling good for you?
Using foam rollers the correct way can help increase flexibility, improve joint range-of-motion, relieve back pain, improve blood flow, and help reduce muscles soreness from post-workout DOMS. These are all reported benefits from regular foam rolling. If you’ve been using a roller for a while, you’ll have already noticed the positive changes. You might also be wondering why so many people are torturing themselves in the name of health. But foam rolling should be no more painful than a firm massage. If you grit your teeth as you roll down your IT band for the hundredth time, stop right there. We’ll talk about how to use one properly but for now, let’s look at why you should use a roller.

Why should you be foam rolling?
- Flexibility – Foam rolling has been shown to significantly improve flexibility, especially when combined with a typical warm-up routine before exercise (1). And the good news is you don’t need to roll it ‘til it hurts; studies have shown this improvement after just 2 minutes of rolling the specific area (2). So whether you’re looking to work on the flexibility in yoga, or just looking to loosen those stiff joints, reaching for the foam roller is a good idea.
- Performance – When it comes to pre-workout warm-up, you might think back to school days of standing around doing a few static leg stretches. As it turns out, those static stretches actually reduce the endurance and strength of muscles immediately after stretching (3). Not ideal if you’re about to do a heavy set of squats! Fortunately, foam rolling has no such negative side effects! Next time you warm-up for the squat rack, try a few minutes of rolling the hip flexors, quads and glutes and leave the static stretching for after your workout.
- Recovery – Post-workout foam rolling has become a staple for many athletes and for good reason. Foam rolling has been shown to substantially reduce the amount of soreness associated with DOMS and help your muscles recover faster (4). That’s a Win-Win situation.

What about back pain?
Mild back pain is often due to overuse or and imbalance of muscles. For this sort of problem, foam rolling can be a great tool to help relieve tightness. However, there are many reasons for back pain and not all of them should be treated with the roller. Figuring out when you should and shouldn’t use a roller can be difficult. The best course of action is to check with your practitioner.
How do I use a foam roller?
This is a really common question. Luckily it’s not hard to learn how to use a foam roller. After consulting with your osteopath, they might recommend you foam target a particular muscle or muscle group. They can show you exactly how to “roll” these areas. (At MetaMed, we have some handy printouts with diagrams in case you forget).
CLICK HERE TO GET YOUR FOAM ROLLER EXERCISES
When rolling any part of the body, there is a sweet spot of pressure for the best results; too much or too little and you won’t get the maximum benefit. All parts of the body are not equally receptive. Some areas can have trigger points or tighter muscles that can feel more painful than others.
We recommend finding a pressure you can work with for 2 minutes. It should allow you to relax. Your muscles will be tight when you begin but should relax by the time you’ve finished. If not, and you’re still feeling discomfort, you might be using too much pressure. In terms of frequency and duration, 3 to 4 times a week works for most people and approximately 2-3 minutes for each area.
I’m a runner, do I need to roll more often than most?
Runners will benefit from around 3 times a week but avid runners doing long-distance training might want to get an extra rolling session done. Pay attention to the IT band. Many runners live in fear of IT band syndrome. This painful condition affects the knee and sometimes the hip. Pain is felt when the IT band rubs over bony areas, causing inflammation during the running motion. The syndrome is often associated with tightness of the IT band. In the early days of foam rolling, this thinking led to runners spending hours a week rolling up and down this painful band of tissue.
While more rolling may sound like a good idea, the reason we call it a “band” and not a muscle is because it’s simply not a muscle. In fact, it’s technically a tendon. And tendons can’t be stretched. If you’re worried about ITB syndrome or already have it, there are ways to address it without torturing yourself on the roller!

What kind of roller do I need?
Foam rollers come in a variety of sizes, textures, and densities. Like most products these days there is an abundance of choice. We recommend picking a medium-soft one for beginners with a relatively smooth surface. Experienced users might prefer firmer ones that can come with spikes and nodules that help get into the hard-to-reach places. Note that these products can be seriously uncomfortable for the majority of people.
Is there anything I should watch out for when using my roller?
On the whole, foam rolling is a very safe practice provided it’s used carefully. Roll muscles only. Avoid bony bits, rolling over joints, or the site of a recent injury. If it’s really sore or painful, stop and ask us about it!
- Mohr, A., Long, B. and Goad, C. (2014). Effect of Foam Rolling and Static Stretching on Passive Hip-Flexion Range of Motion. Journal of Sport Rehabilitation, 23(4), pp.296-299.
- MacDonald, G., Penney, M., Mullaley, M., Cuconato, A., Drake, C., Behm, D. and Button, D. (2013). An Acute Bout of Self-Myofascial Release Increases Range of Motion Without a Subsequent Decrease in Muscle Activation or Force. Journal of Strength and Conditioning Research, 27(3), pp.812-821.
- NELSON, A., KOKKONEN, J. and ARNALL, D. (2005). ACUTE MUSCLE STRETCHING INHIBITS MUSCLE STRENGTH ENDURANCE PERFORMANCE. Journal of Strength and Conditioning Research, 19(2), pp.338-343.
- Lane, J., Kripaitis, D. and Spina, M. (2017). The effect of Foam Rolling (FR) on recovery from delayed onset muscle soreness. Physiotherapy, 103, p.e46.
Foam roller
The post Are Foam Rollers Worth it? Why & How to use a Massage Roller appeared first on MetaMed.
]]>